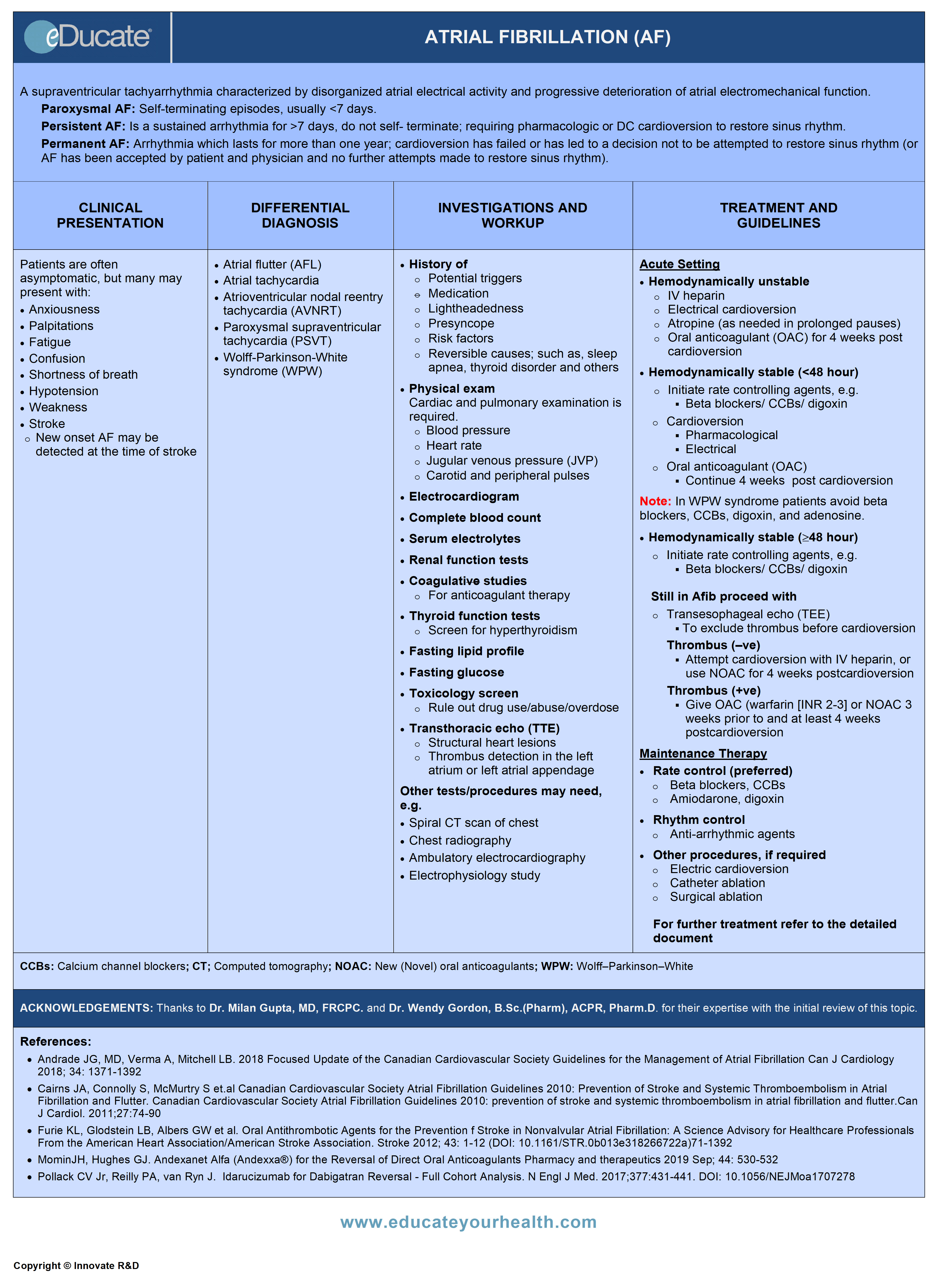
Atrial Fibrillation (AF)
ACKNOWLEDGEMENTS:
Thanks to Dr. Milan Gupta, MD, FRCPC, Associate Clinical Professor of Medicine, McMaster University, Staff Cardiologist, William Osler Health System, Brampton, ON Canada, and Dr. Wendy Gordon, B.Sc.(Pharm), ACPR, Pharm.D., Clinical Pharmacy Specialist, Fraser Health Authority (Royal Columbian Hospital), New Westminster, BC Canada for their expertise with the initial review of this topic.
[pdf-embedder url=”https://www.educateyourhealth.com/wp-content/uploads/2019/03/AF-Brochure-.pdf” width=”750″]
Definition
Atrial fibrillation (AF): Supraventricular tachyarrhythmia characterized by disorganized atrial electrical activity and progressive deterioration of atrial electromechanical function.
Classified as:
- Paroxysmal AF: Self-terminating episodes, usually <7 days
- Persistent AF: Sustained arrhythmia for >7 days, do not self-terminate; requiring pharmacologic or DC cardioversion to restore sinus rhythm
- Permanent AF: Arrhythmia which lasts for more than one year; cardioversion has failed or has led to a decision not to be attempted to restore sinus rhythm (or AF has been accepted by patient and physician and no further attempts made to restore sinus rhythm
Ref: Healey JS et al. Canadian Journal of Cardiology 2011; 27: 31-37

Etiology
- Cardiac and Pulmonary disease
- Hypertension
- Coronary artery disease (CAD)/ myocardial infarction (MI)
- Congenital/structural heart disease
- Valvular heart diseases i.e. mitral regurgitation and aortic stenosis
- Supraventricular tachyarrhythmia’s including (Wolff-Parkinson-White syndrome, atrial flutter and tachycardia)
- Previous heart surgery
- Sick sinus syndrome
- Cardiomyopathy/ myocarditis/ pericarditis
- Chronic obstructive pulmonary disease (COPD)/ pneumonia
- Pulmonary embolism or hypertension
- Drug use
- Alcohol/ cocaine/ caffeine
- Methamphetamines
- Digoxin toxicity
- Endocrine disorders
- Hyperthyroidism
- Pheochromocytoma
- Neurogenic
- Subarachnoid hemorrhage
- Large ischemic stroke
- Familial atrial fibrillation
- Lone (idiopathic) AF: Lone AF describes paroxysmal, persistent, or permanent atrial fibrillation in patients without underlying pathology
- Other:
- Obesity/ obstructive sleep apnea
- Vagally medicated (habitual aerobic training)
Epidemiology
Prevalence and incidence increases with age.
Estimated Prevalence:
Approximately 1% of the general population has 1 in 4 lifetime risk of developing AF.
Distribution of prevalence according to the age is as follows:
- <60 years of age 0.1%
- 60-80 years of age 1-4%
- >80 years of age 9%
Estimated Incidence:
- ≤50 years of age 0.5%/1000/year
- ≥70 years of age 9.7/1000/year
Gender predominance: Male > Female
Overall AF affects: Approximately 200,000 to 350,000 Canadians and 2.2 million Americans.
Ref: Heart and stroke foundation statistics
Pathophysiology
Genesis of atrial fibrillation (AF):
- Usually involves foci of cells in the left atrium in vicinity of the pulmonary vein
- Increased adrenergic discharges stimulate these cells (rapid firing) which are followed by a vagal response
- Subsequent generation of a multitude of atrial wavelets → nonhomogeneous conduction in the left atrium → intraatrial reentry phenomenon and continuation of atrial fibrillation (AF)
Mechanism of thromboembolism:
- Stasis → clot formation → embolization
Clinical Presentation
- Often asymptomatic; diagnosed incidentally on a routine examination
- Palpitations/ fatigue/ anxiety
- Shortness of breath/ chest pain
- Hypotension/ lightheadedness/ confusion
Symptoms secondary to cardioembolism:
- Stroke or transient ischemic attack (TIA)
- Ischemic limb (cold pulseless limb)
- Ischemic bowel (abdominal pain, discomfort)
Note: Risk of cardioembolism is the same whether permanent or paroxysmal atrial fibrillation (PAF).
Differential Diagnosis
- Atrial flutter (AFL)
- Atrial tachycardia
- Atrioventricular nodal reentry tachycardia (AVNRT)
- Paroxysmal supraventricular tachycardia (PSVT)
- Wolff-Parkinson-White syndrome (WPW)
Investigation and Workup
History:
- Identify reversible causes (e.g. hyperthyroidism, ventricular pacing, exercise, etc.)
- Identify risk factors (e.g. hypertension, sleep apnea)
- History of potential triggers (e.g. alcohol, intensive aerobic training)
- Family history of atrial fibrillation (particularly lone AF)
- Medication history for atrial fibrillation, both for efficacy and adverse effects
- History of lightheadedness/ presyncope
Physical:
Full cardiac and pulmonary exam is valuable in reaching a definitive diagnosis and includes the following:
- Blood pressure, pulse and respiratory rate, including height and weight
- Obesity predisposes to sleep apnea; both are associated risk factors, which should be treated with lifestyle changes
- Jugular venous pressure, carotid and peripheral pulses should be checked
Laboratory:
- Complete blood count
- Coagulation (PTT, INR)
- Serum electrolytes
- Renal function tests
- Liver function tests
- Thyroid function tests
- Fasting lipid profile
- Fasting glucose
- Toxicology screen
- 12 lead electrocardiogram (ECG)
Imaging studies may include:
- Transthoracic echocardiogram/Transesophageal echocardiogram (TTE/TEE)
- Chest radiography
- To rule out cardiopulmonary diseases and cardiomyopathies
- Ambulatory blood pressure monitoring
- In case of borderline hypertension
- Electrophysiology study
- In patients with documented regular supraventricular tachycardia for catheter ablation
- Sleep study
- For patients with symptoms of obstructive sleep apnea
Treatment
-
- Treatment of atrial fibrillation (AF) focuses on ventricular rate and rhythm control, along with prevention of thromboembolism
- Primary goal:
- Amelioration of symptoms
- Prevent recurrent arrhythmias
- Prevent stroke and cardiomyopathy
1. Hemodynamically unstable:
- Electric cardioversion (defibrillation)
- Start with 150-200 joules biphasic waveform in synchrony with the R wave
- IV Heparin
- 60 units/kg loading dose followed by 12 units/kg per hour to maintain an aPTT of approximately 1.5-2 times the control value
- Low molecular weight heparin (LMWH) may also be used
- Atropine (1 mg IV) should be readily available to treat prolonged pauses
Note: Anticoagulation should be used in this setting. particularly for AF of unknown duration (or ≥48hr) or if patient is at high risk of stroke (mechanical or valvular heart disease, previous TIA or stroke). Unless contraindicated all patients require ≥4 weeks of oral anticoagulation post cardioversion.
2. Hemodynamically stable (AF or atrial flutter duration <48 hours)
In selected patients, initial therapy with rate slowing agent is acceptable while waiting for spontaneous cardioversion, such as
- Beta-blockers
- Calcium channel blockers (CCBs)
- Digoxin (second-line therapy)
Ref: Ian G. Stiell et al. Canadian Journal of Cardiology 2011; 27: 38-46.
Caveat: In special circumstances like Wolff-Parkinson-White syndrome (presence of an extra, abnormal electrical pathway in the heart leading to tachycardia), avoid beta blockers, CCBs, digoxin, and adenosine; consider intravenous anti-arrhythmic e.g.
- Procainamide: 15-18 mg/kg IV over 60 min slow infusion
- Ibutilide: 1-2 mg IV over 10-20 min; pretreat with MgSO4 1-2 mg IV
If the patient is still in AF, cardioversion without prior anticoagulation may be considered in low-risk patients <48h
a) Pharmacological cardioversion:
Class Ia:
- Procainamide: 15-17 mg/kg IV over 60 min
Class Ic:
- Propafenone (oral): 450 mg (wt. <70 kg); 600 mg (wt. ≥70 kg)
- Flecainide (oral): 200 mg (wt. <70 kg); 300 mg (wt. ≥70 kg)
Class III:
- Ibutilide: 1-2 mg IV over 10-20 min; pretreat with MgSO4 1-2 mg IV
Note: Class Ic drugs (propafenone, flecainide ) should be used in combination with AV nodal blocking agents (beta-blockers or calcium-channel blockers) to avoid paradoxical increase in ventricular rate due to the drug-induced conversion of atrial fibrillation (AF) to atrial flutter (AFL). Class Ic should also be avoided in patients with structural heart disease.
b) Electrical cardioversion:
Recommended in case of pharmacological cardioversion failure.
- Prophylactic anti-arrhythmic drugs before electrical cardioversion in the emergency department are recommended in order to decrease early recurrence of AF or AFL and to enhance cardioversion efficacy
Ref: Ian G. Stiell et al. Canadian Journal of Cardiology 2011; 27: 38-46
c) Oral anticoagulant (OAC):
- For high-risk patients (e.g. valvular heart disease, recent stroke/TIA) OAC uses for 3 weeks prior to cardioversion is recommended. In addition, OAC is recommended for ≥4 weeks of post cardioversion. Antithrombotic therapy with OAC or Acetylsalicylic acid (ASA) is then based on the risk of recurrent AF and CHADS2 score

3. Hemodynamically stable (AF or AFL duration ≥48 hours)
- Start with rate slowing agents (beta blockers, CCBs, and digoxin)
- If there is no optimal response with rate slowing therapy, then consider cardioversion
- Perform ECHO (TEE or TTE) to exclude thrombus before cardioversion
- If no thrombus, then start cardioversion (preferably electric cardioversion) with IV heparin or NOAC therapy thereafter for at least 4 weeks
- If thrombus is present or ECHO is not available then give OAC (warfarin [INR 2-3] or NOAC for 3 weeks before and at least 4 weeks post cardioversion
- Prophylactic treatment with antiarrhythmic drugs is advisable after cardioversion in high-risk patients, in view of high relapse
Ref: Ian G. Stiell et al. Canadian Journal of Cardiology 2011; 27: 38-46.
Special considerations:
Cardioversion in patients with implanted pacemakers and defibrillators
- The electrode paddle should be at least 8 cm away from the pacemaker battery
- Anteroposterior paddle positioning is recommended
- Biphasic shocks are preferred
- After cardioversion, the device should be evaluated to ensure normal function
AV junction ablation and implantation of a permanent pacemaker
- Indicated in symptomatic patients with uncontrolled ventricular rates during atrial fibrillation despite maximally tolerated combination pharmacologic therapy
Maintenance Therapy
- Rate control
- Rhythm control
- Thromboembolic prophylaxis
1) Rate Control
Beta blockers, calcium channel blockers (CCBs):
- Usually first line rate control agents in most patients without past history of myocardial infarction (MI) or left ventricular dysfunction (LVD)
Digoxin:
- IV: 0.5-1 mg; usual dose 0.1-0.4 mg IV once daily
- Oral: 0.75-1.5 mg PO; usual dose 0.125-0.5 mg once daily
- Not to be used for initial therapy in active patients; usually used as initial therapy in patients who are sedentary or who have left ventricular systolic dysfunction.
- May be used as an adjunct with beta blockers or CCBs in whom rate control is not achieved.
Amiodarone:
- 400 mg PO TID over 5-7 days, then 400 mg/day over 1 month, then 200 mg/day
- Usually reserved when other means are not feasible or are insufficient for rate control (because of adverse effects).
Dronedarone:
- 400 mg PO BID with meals
- Indicated for treatment of patients with non-permanent AF
- Reduces hospitalizations due to AF
- May be used as an adjunct with beta-blockers, calcium channel blockers and used with caution with digoxin, if ventricular rate is uncontrolled despite therapy
- Requires regular monitoring of liver function
HOWEVER, this agent is now contraindicated in:
- Permanent AF, duration at least 6 month
- Severe heart failure (NYHA stage IV) or unstable hemodynamic conditions
- Left ventricular ejection fraction (LVEF) <40%
- 2nd or 3rd degree AV block or sick sinus syndrome (SSS); unless functioning pacemaker present
Catheter ablation:
-
- Atrioventricular (AV) junction ablation and permanent pacemaker implantation may be employed in those refractory to maximum combined medical therapy
- OAC therapy be continued following AF ablation in patients with
- i) CHADS2 score ≥1
- ii) Mechanical heart valve
2) Rhythm Control
Anti-arrhythmic agents in maintenance therapy:
Generally reserved for patients with AF or AFL who remain symptomatic with rate control therapy or in whom rate control therapy is unlikely to control symptoms, agents used include:
Propafenone or Flecainide – Class I:
- Used with structurally normal heart
- Fast onset of action
Sotalol – Class III:
- Avoid in decompensated congestive heart failure
- Not very effective in converting recent onset AF to sinus rhythm
Dofetilide – Class III:
- Not available in Canada
Amiodarone – Class I, II, III, and IV:
- Effective but has extensive toxicity
- Used in those with severely depressed LV function
- Usually indicated in patients with recent-onset AF and structural heart disease
Dronedarone – Class III:
- Initially considered less toxic, but also less effective than amiodarone and is used to lower side effects with acceptance of higher recurrence of AF
- Contraindications: Permanent AF/severe heart failure/LVEF <40% / 2nd or 3rd degree AV block (as discussed in rate control above)
“Pill in the Pocket” for selected patients with atrial fibrillation
- Self-treatment with intermittent antiarrhythmic drug therapy (propafenone or flecainide) is usually recommended; as an alternative to daily antiarrhythmic therapy, in symptomatic patients with infrequent long-lasting episodes of AF
Caveat: Avoid oral antiarrhythmic therapy in patients with AF/AFL or advanced sinus or AV nodal disease unless pacemaker or defibrillator has been installed.
(prevention of thromboembolic complications and bleeding risk)
a) Patients with AF often require prophylaxis with anticoagulant therapy, unless contraindicated
Therapeutic choices include:
- IV heparin/low-molecular-weight heparin (LMWH) (may be considered for short-term prophylaxis)
- NOACs
- Apixaban
- Dabigatran
- Edoxaban
- Rivaroxaban
- Warfarin
The therapy, in turn, is based on clinically relevant thromboembolic risk factors which are summarized as follows:
Major risk factors are considered:
- Previous stroke, transient ischemic attack (TIA)
- Previous systemic embolism
- Age >65 years
Clinically relevant non-major risks:
- Heart failure or severe to moderate LV systolic dysfunction (e.g. LVEF <40%)
- Hypertension
- Diabetes mellitus
- Female sex
- Age 65-74 years
- Vascular disease
b) The risk/benefit ratio for patient selection has been outlined in number of scales/tools, which have been summarized in one table for convenience
c) Based upon the therapeutic bleeding risk stratification scores (HAS-BLED score) in AF:
- Patients with HAS-BLED Score ≥3 indicates increased one-year bleeding risk on anticoagulation, sufficient enough to justify caution or more regular review.
d) Concomitant AF and Non-ST elevation acute coronary syndromes (NSTEACS) or STEMI:
- Up to 20%-30% of AF patients also have concomitant CAD, with the conundrum being that OAC is superior to antiplatelet therapy for prevention of cardiac embolism, while DAPT is more effective than an OAC alone in reducing ischemic coronary events in ACS patients while triple therapy (TT) – OAC + DAPT increase risk of major bleeding. The decision to use various combinations of antithrombotic therapy, therefore, requires careful consideration of risk of recurrent MI and systemic embolism/stroke versus risk of bleeding
- Every effort should be made to aggressively manage modifiable bleeding risk factors to help mitigate risk of bleeding from combined OAC + APT therapy, e.g. monitor and treat anemia, thrombocytopenia, avoid use of NSAIDS, prasugrel and ticagrelor and consider use of proton pump inhibitor use; target lower INR range (eg, 2.0-2.5) for those on warfarin
e) Concomitant NVAF and percutaneous coronary intervention (PCI):
- NVAF + ACS in a patient is aged < 65 years with no CHADS2 risk factors:
-
- No PCI: ASA + Clopidogrel or Ticagrelor for 12 months then continues ASA alone
- With PCI: ASA + Clopidogrel or Ticagrelor or Prasugrel for 12 months then continues ASA alone
- NVAF with CAD or PAD aged ≥65 or the CHADS2 score ≥1:
- ACS without PCI: Clopidogrel 75 mg/d + OAC for 12 months post-PCI then continue OAC alone
- Elective PCI without high risk features for thrombotic cardiovascular events: Clopidogrel 75 mg/d + OAC for at least 1 month with bare metal stent and at least 3 months with drug eluting stent up to 12 months post-PCI then continue OAC alone
- ACS with PCI or elective PCI with high risk features for thrombotic cardiovascular events: Triple antithrombotic therapy with ASA 81 mg/d + Clopidogrel 75 mg/d + OAC for 6 months followed by Clopidogrel + OAC up to 12 months after ACS then continue OAC alone
f) Special considerations in the patient who are on prevention of thromboembolic complication:
Subclinical Atrial Fibrillation (SCAF):
- Appears to have a lower risk of stroke as compared to those with clinical AF
- Uncertainty remains regarding the duration AF above which stroke risk is increased
- OAC therapy may be considered for patients >65 years or CHADS2 score >1 with episodes of SCAF lasting > 24 hours, or for shorter episodes in high-risk patients (such as those with a recent cryptogenic stroke)
Patients on antiplatelet therapy or OAC scheduled for surgery:
Note: Most procedures with a low risk of bleeding, such as cardiac device implantation and most dental procedures can generally be safely performed without interrupting anticoagulant therapy, provided the INR is not supratherapeutic in the case of warfarin
Ref: Macle L, Cairns J, Leblanc K et al. Canadian Journal of Cardiology 2016; 32: 1170-1185.


Bleeding complications from OAC:
Hold OAC, ensure hemodynamic stability.
Reversal Agents for NOACs:
Dabigatran – Idarucizumab:
- Specific reversal agent for dabigatran, complete reversal is expected within minutes
- Administered as two 50‐mL bolus infusions containing 2.5 g each of idarucizumab (total 5 g) no more than 15 minutes apart
Factor Xa Inhibitors (Apixaban, Edoxaban, Rivaroxaban) – Andexanet Alfa:
- Low-dose regimen – 400-mg IV bolus administered 30 mg/ min, followed by a two-hour IV infusion at a rate of 4 mg per minute
- High dose regimen – 800-mg IV bolus administered 30 mg/min, followed by a two-hour IV infusion given at a rate of 8 mg per minute
Other consideration for life-threatening DOAC bleed:
- Prothrombin complex concentrate (PCC), or Activated prothrombin complex concentrate (aPCC)
- Tranexamic acid
- Hemodialysis
Procedures
1) Electric cardioversion:
- Safe and effective method for quick restoration of sinus rhythm:
- If AF <48 hrs proceed with cardioversion
- If AF ≥48 hrs or of unknown duration anticoagulant therapy is suggested (see “Hemodynamically Stable AF or AFL duration 48 hr” section above)
- Biphasic external defibrillators are preferred
- Start with a lower possible dose in small size patient
- Electrode placement positions:
- Anteroposterior electrode placement (more effective)
- Anterolateral placement
- If initial shocks are unsuccessful:
- Reposition electrodes and repeat cardioversion
- Outpatient/ambulatory cardioversion can be undertaken:
- In hemodynamically stable with no underlying severe heart disease
- Post-procedure monitoring:
- Blood pressure, heart rate and telemetry for ≥3 hrs
2) Catheter ablation:
- Is chosen as first-line therapy in highly selected patients with symptomatic paroxysmal AF
- AF ablation should not be considered as an alternative to oral anticoagulation, and initiation of anticoagulation should not be delayed in patients with high thromboembolic risks
Potential sites for ablation:
a) Accessory pathway
- Indicated in patients with evidence of ventricular pre-excitation during AF, such as rapid ventricular rates, syncope
- Definitive therapy for patients with Wolff-Parkinson-White syndrome
b) AV node ablation and implantation of a permanent pacemaker
- For those with uncontrolled ventricular rates refractory to maximal pharmacologic therapy, a pacemaker and indefinite anticoagulant therapy is often required
c) Left atrial catheter ablation
- Effective for either paroxysmal or chronic AF
d) Pulmonary vein isolation ablation (PVI ablation or PVA)
- Effective in patients who have “paroxysmal” AF
3) Surgical ablation:
Usually reserved for those patients who have failed a catheter ablation strategy or who have planned concomitant cardiac surgery.
Procedures usually used are:
- Maze procedure
- Cox Maze III procedure
- Minimally invasive surgical ablation (e.g.)
- Wolf Mini Maze
- Saltman Microwave Mini Maze
[/cq_vc_tab_item][cq_vc_tab_item tabtitle=”Medication Dose”]RATE CONTROL:
Beta-adrenergic blocking agents
- Cardioselective
- Atenolol
- Esmolol
- Metoprolol
- Non-cardioselective
- Propranolol
- Sotalol
Mechanism:
- Block Beta receptors
- Decrease heart rate and cardiac output
- Decrease renin release
Dose: Cardioselective
Atenolol:
Atrial fibrillation
- 2.5-5 mg slow IV infusion over 2-5 minute; Max. 10 mg over 10-15 minute
Esmolol:
SVT/Postoperative tachycardia/Hypertension (gradual control)
- 500 mcg/kg IV over 1 minute; then 50 mcg/kg/minute infusion over 4 min; Max of 300 mcg/kg/min
- Titration: Increased by 50 mcg/kg/minute (once in 4 mins) as needed
- Note: If no response within 5 minutes, may give 2nd loading dose of 500 mcg/kg over 1 minute, then 100 mcg/kg/minute infusion over 4 minute
Intraoperative tachycardia/Hypertension (immediate control)
- 1.5 mg/kg IV bolus over 30 sec.; Then 0.15 mg/kg/minute infusion, if necessary; Max. 0.3 mg/kg/minute
Metoprolol:
Atrial fibrillation/Supraventricular tachycardia
- Acute treatment: 2.5-5 mg IV every 2-5 minutes; Max. 15 mg over 10-15 minute
- Maintenance (immediate release): 25-100 mg PO BID
Dose: Non-cardioselective
Propranolol:
Tachyarrhythmias
- Intravenous: 1-3 mg slow IV push every 2-5 mg up to total of 5 mg
- Regular Tablet: 10-30 mg PO QID or TID
Sotalol: (antiarrhythmic agent class III & II)
- 40-160 mg PO twice daily; usual initial dose can be 80 mg PO twice daily, if required may go up to 240-320 mg PO per day
Calcium channel blocking agents (CCBs)
- Diltiazem
- Verapamil
Mechanisms:
- Blocks calcium influx by binding to the L-type calcium channels in the heart and in smooth muscle of the peripheral vasculature
- Decreases intracellular calcium leading to a reduction in muscle contraction
- Significant reduction in afterload, with no effect on preload
Dose: Non-Dihydropyridines
Diltiazem:
Supraventricular tachyarrhythmias
- 0.25 mg/kg IV over 2 minute; if desired response not achieved in 15 minutes, may repeat 0.35 mg/kg IV bolus over 2 minute; then follow with continuous infusion at 10 mg/hr (range 5-15 mg/hr) for up to 24 hr, if required
- Note: Infusions >24 hrs or >15 mg/hr are not recommended
Verapamil:
Chronic atrial fibrillation/PSVT (prophylaxis)
- Immediate-release: 240-480 mg/day PO divided in 3-4 doses; usual 120-360 mg/day in 3-4 divided doses
Supraventricular tachyarrhythmias
- Dosage: 2.5-5 mg IV over 2 minutes; may repeat 5-10 mg IV 15-30 minute after the initial dose if required; Max. 20-30 mg
RHYTHM CONTROL
- Class Ia
- Procainamide
- Class Ic
- Propafenone
- Flecainide
- Class III
- Ibutilide
- Amiodarone
- Ibutilide
Mechanisms:
- Complete mechanism of antiarrhythmic action is not known
- Depress Na conductance and block K+ channel → resulting in increased action potential duration (APD) and effective refractory period (ERP)
- Ic agents block Na+ channels more potently than the Ia drugs and have some beta-blockade activity
Dose: Class Ia:
Procainamide:
Atrial Fibrillation
- Initial loading dose: 15-17 mg/kg slow infusion over 60 minutes or 100 mg/dose repeated every 5 minutes (rate not to exceed 50 mg/minute) to a total dose of 1 g
- Maintenance: 1-4 mg/minute IV continuous infusion
- Oral: Initially 1.25 g PO; followed by 0.75 g PO after 1 hour interval. If there is no change on ECG, give additional doses of 0.5-1 g every 2 hours until arrhythmia is interrupted or until toxic effects appear
- Maintenance (extended-release): Up to 50 mg/kg/day PO in equally divided doses every 6 hrs starting 2 to 3 hours after the last dose of conventional tablets
Hemodynamically stable monomorphic VT/Pre-excited atrial fibrillation (ACLS)
- Loading dose as IV Infusion 20-50 mg/minute Or 100 mg every 5 minutes (rate not to exceed 50 mg/minute), until the arrhythmia is suppressed, a fall in BP of >15 mmHg occurs, excessive widening of the QRS complex (≥50%) from baseline or prolongation of the PR interval occurs, severe adverse effects appear, or a total dose of 17 mg/kg is given
- Maintenance: Followed by continuous infusion of 1-4 mg/minute
Dose: Class Ic
Propafenone:
Paroxysmal atrial fibrillation (“Pill-in-the-pocket”)
- Weight <70 kg: 450 mg PO
- Weight ≥70 kg: 600 mg PO
- Avoid repeating in ≤24 hrs
Recent onset atrial fibrillation
- 150 mg PO given every 8 hours (total of 450 mg/day). May increase in 3-4 days interval to 300 mg PO every 12 hours (total of 600 mg/day) and if required may increase dose to 300 mg PO every 8 hours (900 mg/day)
Flecainide:
Prevention of PSVT/Paroxysmal atrial fibrillation
- 50 mg PO BID, may increase by 50 mg PO BID at 4 day intervals; Max. 300 mg/day
Paroxysmal atrial fibrillation – “pill-in-the-pocket” dose
- Weight <70 kg: 200 mg PO daily; weight ≥70 kg: 300 mg PO daily
Note: Patient must be on an AV nodal-blocking agent prior to initiation of antiarrhythmic. No more than one dose during a 24-hour period.
Dose in renal impairment:
- If CrCl <35 ml/minute, initiate 100 mg PO daily OR 50 mg PO BID: may increase dose at 4 day intervals cautiously, if needed
Dose: Class III
Ibutilide:
Atrial fibrillation/flutter
- <60 kg: 0.01 mg/kg IV infusion over 10 minutes
- ≥60 kg: 1 mg IV infusion over 10 minutes
Note: May repeat 2nd dose after 10 minutes
Atrial fibrillation/flutter after cardiac surgery
- <60 kg: 0.005 mg/kg over 10 minute; ≥60 kg: 0.5 mg IV infusion over 10 minutes
- Note: May repeat one additional time. If arrhythmia terminates discontinue the infusion
Amiodarone:
Atrial fibrillation pharmacologic cardioversion
- 5-7 mg/kg IV over 30-60 minutes; followed 1.2-1.8 g/day IV continuous infusion or PO in divided doses until total of 10 g
- Maintenance: 200-400 mg/day in divided or single dose
- Inpatient: 1.2-1.8 g PO daily in divided doses up to a total of 10 g
- Maintenance: 200-400 mg/day PO in divided or single dose
- Outpatient: 600-800 mg PO in single or divided dose; up to a total of 10 g
- Maintenance: 200-400 mg/day in divided or single dose
Recurrent atrial fibrillation
- 10 mg/kg/day PO in single or 2 divided doses for 14 days; then 300 mg PO daily for 4 weeks, followed by of 200 mg PO daily for maintenance OR
- 400 mg PO TID for 5-7 days; then 400 mg /day for 1 month; followed by 200 mg/day
Dronedarone:
Atrial fibrillation/Flutter
- 400 mg PO BID with meals
- Digoxin
Mechanisms:
Exact mechanism of action not known; however, the acceptable hypothesis is as follows:
- Inhibition of the sodium/ potassium ATPase pump in myocardial cells results in a transient increase of intracellular sodium, which in turn promotes calcium influx via the sodium-calcium exchange pump leading to increased contractility
- There is a direct effect on the conductivity of A-V node which is delayed; slowing the rate of origin of impulses from the S-A node. In short heart rate becomes slow. These effects are largely due to parasympathetic stimulation
Dose:
Digoxin:
AF + Heart failure
- Acute management: Loading dose 250 mcg IV (0.25 mg) every 2 hours up to total of 1500 mcg (1.5 mg) in a day
- Non-acute management: 500 mcg (0.5 mg) PO daily for 2 day
- Maintenance: 125-375 mcg (0.125-0.375 mg) IV/PO daily
Supraventricular tachyarrhythmia
Total digitalizing dose (TDD)
- 500-1000 mcg (0.5-1 mg) IV/IM; start with 50% of the TDD, then one-quarter of the TDD in each of 2 subsequent doses at 6-8 hr intervals
- 750-1500 mcg (0.75-1.5 mg) PO; start with 50% of the total digitalis dose (TDD), then one-quarter of the TDD in each of 2 subsequent doses at 6-8 hr intervals
- Note: Obtain ECG 6 hours after each dose to assess potential toxicity.
Daily maintenance dose
- 125-500 mcg (0.125-0.5 mg) PO daily
- 100-400 mcg (0.1-0.4 mg) PO daily
Note: Intramuscular injections are not preferred due to severe pain at the site of injection.
CARDIOEMBOLIC PROPHYLAXIS
- Heparin (unfractionated)
- Low-molecular-weight heparin (LMWHs)
- Enoxaparin
- Dalteparin
- Oral anticoagulants (OAC)
- Warfarin
- NOAC/DOAC
- Apixaban
- Dabigatran
- Edoxaban
- Rivaroxaban
Mechanism:
- Inhibits thrombus formation and prevent extension of existing thrombi
- No direct lytic effect on established thrombi
- Prolongs aPTT, PT and INR
Dose:
Typical use for IV heparin
Symptomatic AF with consideration of cardioversion or thrombus detection on ECHO
AF with concomitant TIA or minor/small ischemic stroke
- Initial IV bolus of ~60-80 IU/kg or 5000 IU
- Followed by an infusion of 12 IU/kg/hr; Max. 1000 IU/hr
- Adjusted to maintain an APTT to 1.5-2 times normal (usually 50 to 70 seconds)
Caveat: For patients with moderate or large strokes, the above may be modified to a low initial exposure for the avoidance of supra-therapeutic PTT and potential risk of bleeding:
- Initial IV bolus of ~30-40 IU/kg or 2500 IU or no bolus
- Followed by an infusion of 12 IU/kg/hr; Max. 1000 IU/hr
- Adjusted to maintain an APTT to 1.4-1.8 times normal (suggested, but adjusted at the discretion of treating physician)
Low-molecular-weight heparin (LMWH):
May sometimes be used for patients with AF/AFL
- Enoxaparin: 1 mg/kg every 12 hrs
- Dalteparin: 200 IU/kg/day SC every 12 hrs or once daily
Warfarin:
Prevention/treatment of thrombosis/embolism
- Start 2-10 mg PO once daily for 1-2 days then adjust dose according to INR results
- Desired INR 2-3 for nonvalvular atrial fibrillation/flutter or INR 2.5-3.5 if concomitant mechanical mitral valve
- Warfarin dose-Suggested protocol for adults with AF (No Mechanical Valve)
- Warfarin dose-Suggested protocol for patients with mechanical valves ±AF
- Warfarin reversal-Suggested protocol
Dabigatran:
Dose (Canada labelling):
- Age <80 year: 150 mg PO BID if creatinine clearance >30 ml/minute
- Age >80 years: 110 PO BID if creatinine clearance >30 ml/minute
- Contraindicated in creatinine clearance <30 ml/minute
Dose (USA labelling):
- 150 mg PO BID if creatinine clearance >30ml/minute
- 75mg PO BID if creatinine clearance 15-30 ml/minute
Conversion from dabigatran to parenteral anticoagulant
- Wait 12 hrs. after the last dose of dabigatran before switching to a parenteral anticoagulant
Conversion from vitamin K antagonists (e.g. warfarin) to dabigatran
- Dabigatran should only be started after vitamin K antagonists have been discontinued, and the patient’s INR <2.0
Conversion from dabigatran to vitamin K antagonists (e.g. warfarin)
- Stop dabigatran for 12 hrs then begin warfarin protocol/nomogram (see above)
Rivaroxaban:
- GFR ≥50 ml/minute: 20 mg PO daily
- GFR 30-49 ml/minute: 15 mg PO daily
Apixaban:
- GFR >25 ml/minute: 5 mg PO BID; alternatively, 2.5 mg BID may be considered in patients with at least 2 of the following features: Age ≥80 years, body weight ≤60 kg, or serum creatinine ≥133 micromole/L (1.5 mg/dL)
Edoxaban:
Prevention of Stroke and Systemic Embolism in Patients with NVAF:
- 60 mg PO once daily for CrCl >50
- 30 mg PO once daily for CrCl 30–49; low body weight ≤60 kg; or concomitant use of P-glycoprotein inhibitors (e.g. erythromycin, cyclosporine, dronedarone, quinidine, or ketoconazole, except amiodarone and verapamil
Prevention of Recurrent DVT and PE:
- 60 mg PO once daily for CrCl >50
- 30 mg PO once daily for CrCl 30–49; low body weight ≤60 kg; or concomitant use of P-glycoprotein inhibitors (e.g. erythromycin, cyclosporine, dronedarone, quinidine, or ketoconazole, except amiodarone and verapamil
- Idarucizumab
Mechanisms:
- Human monoclonal antibody fragment (Fab) that selectively binds to dabigatran and its metabolites with very high affinity
- Prevent dabigatran binding to thrombin and negating its anticoagulant effects
Dose:
Idarucizumab:
- Administered as two 50‐mL bolus infusions containing 2.5 g each of idarucizumab (total 5 g) no more than 15 minutes apart
Modified recombinant FXa protein:
- Andexanet Alfa
Mechanisms:
- An engineered variant of factor Xa, that binds factor Xa inhibitors with high affinity, without promoting further anticoagulant activity
- Can increase thrombin generation and ultimately promote a procoagulant state
Dose:
Andexanet Alfa:
- Low-dose regimen – 400-mg IV bolus administered 30 mg/ min, followed by a two-hour IV infusion at a rate of 4 mg per minute
- High dose regimen – 800-mg IV bolus administered 30 mg/min, followed by a two-hour IV infusion given at a rate of 8 mg per minute
[/cq_vc_tab_item][/cq_vc_tabs]
Clinical Trials
- AFFIRM – A comparison of rate control and rhythm control in patients with atrial fibrillation
- ATHENA – Effect of Dronedarone on Cardiovascular Events in Atrial Fibrillation
- AF-CHF – Rhythm Control versus Rate Control for Atrial Fibrillation and Heart Failure
- AVERROES – Apixaban in Patients with Atrial Fibrillation
- ARISTOTLE – Apixaban versus Warfarin in Patients with Atrial Fibrillation
- RACE– Lenient versus Strict Rate Control in Patients with Atrial Fibrillation
- ACTIVE W – Clopidogrel plus aspirin versus oral anticoagulation for atrial fibrillation in the Atrial fibrillation Clopidogrel Trial with Irbesartan for prevention of Vascular Events (ACTIVE W)
- CTAF – Amiodarone to Prevent Recurrence of Atrial Fibrillation
- Re-LY – Randomized Evaluation of Long Term Anticoagulant Therapy (RE-LY) With Dabigatran Etexilate
- ROCKET AF – Stroke Prevention in Atrial Fibrillation
- EMBRACE – Atrial Fibrillation in Patients with Cryptogenic Stroke
- ENGAGE AF-TIMI 48 – Edoxaban versus Warfarin in Patients with Atrial Fibrillation
Physician Resources
1. Tips for Patient Care
Risk factor management:
- Assess and treat modifiable risk factors for atrial fibrillation (AF) such as (hypertension, diabetes mellitus, coronary artery disease, thyrotoxicosis, mitral stenosis, alcohol, and drug use/abuse etc.)
Medications:
- Advise patient and family members to comply with medication
- Advise for periodical INR assessment for patients receiving warfarin
- Maintain INR 2.0-3.0 for AF and >2.5-3.5 in most patients with mechanical valves with or without AF
- Be aware of drug-drug and drug-food interactions, particularly with patients on warfarin
- Patient and family members should be aware of bleeding complication of anticoagulant therapy
- Make patients aware of sign and symptoms of stroke
- Avoid use of flecainide and propafenone in patients with structural heart disease
- Over-the-counter (OTC) medications, such as nasal sprays and cold remedies, contain substances that can aggravate AF
- Abrupt withdrawal of beta blockers may exacerbate symptoms
- Digoxin clearance is reduced in renal insufficiency and dose adjustment may be required to avoid toxicity
- IV calcium may produce arrhythmias in digitalized patients
Social and Stress factors:
- Include family or social support in lifestyle modification
2. Scales and Tables
References
Core Resources:
- Andrade JG, MD, Verma A, Mitchell LB. 2018 Focused Update of the Canadian Cardiovascular Society Guidelines for the Management of Atrial Fibrillation Can J Cardiology 2018; 34: 1371-1392
- Cairns JA, Connolly S, McMurtry S et.al Canadian Cardiovascular Society Atrial Fibrillation Guidelines 2010: Prevention of Stroke and Systemic Thromboembolism in Atrial Fibrillation and Flutter. Canadian Cardiovascular Society Atrial Fibrillation Guidelines 2010: prevention of stroke and systemic thromboembolism in atrial fibrillation and flutter. Can J Cardiol. 2011;27:74-90
- Canadian Cardiovascular Society Atrial Fibrillation Guidelines 2010: Prevention of Stroke and Systemic Thromboembolism in Atrial Fibrillation and Flutter
- Cairns JA, Connolly S, McMurtry S, Stephenson M, Talajic M. CCS Atrial Fibrillation Guidelines Committee. Canadian Cardiovascular Society Atrial Fibrillation Guidelines 2010: prevention of stroke and systemic thromboembolism in atrial fibrillation and flutter.Can J Cardiol. 2011;27:74-90
- Compendium of Pharmaceuticals and Specialties (CPS). Canadian Pharmacist Association. Toronto: Webcom Inc. 2012
- Day RA, Paul P, Williams B, et al (eds). Brunner & Suddarth’s Textbook of Canadian Medical-Surgical Nursing. 2nd ed. Philadelphia: Lippincott Williams and Wilkins; 2010
- Furie KL, Glodstein LB, Albers GW et al. Oral Antithrombotic Agents for the Prevention f Stroke in Nonvalvular Atrial Fibrillation: A Science Advisory for Healthcare Professionals From the American Heart Association/American Stroke Association. Stroke 2012; 43: 1-12 (DOI: 10.1161/STR.0b013e318266722a)
- Foster C, Mistry NF, Peddi PF, Sharma S, eds. The Washington Manual of Medical Therapeutics. 33rd ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2010
- Gillis AM, Verma A, Talajic M, Nattel S, Dorian P CCS Atrial Fibrillation Guidelines Committee. Canadian Cardiovascular Society Atrial Fibrillation Guidelines 2010: rate and rhythm management. Can J Cardiol. 2011;27:47-59
- Gillis AM, Skanes AC, CCS Atrial Fibrillation Guidelines Committee. Canadian Cardiovascular Society Atrial Fibrillation Guidelines 2010: implementing GRADE and achieving consensus. Can J Cardiol. 2011;27:27-30
- Gray J, ed. Therapeutic Choices. Canadian Pharmacists Association. 6th ed. Toronto: Webcom Inc. 2011
- Healey JS, Parkash R, Pollak T, Tsang T, Dorian P CCS Atrial Fibrillation Guidelines Committee. Canadian Cardiovascular Society Atrial Fibrillation Guidelines 2010: etiology and initial investigations. Can J Cardiol. 2011;27:31-37
- O’Rourke R, Walsh R, Fuster V, eds. Hurst’s the Heart Manual of Cardiology, 12thEdition. New York: McGraw-Hill; 2008
- Katzung BG, Masters SB, Trevor AJ, eds. Basic and Clinical Pharmacology. 11th ed. New York: McGraw-Hill; 2009
- Longo D, Fauci A, Kasper D, et al (eds). Harrison’s Principles of Internal Medicine. 18thed. New York: McGraw-Hill; 2011
- McPhee SJ, Papadakis MA, eds. Current Medical Diagnosis & Treatment. 49th ed. New York: McGraw-Hill; 2010
- Mitchell LB CCS Atrial Fibrillation Guidelines Committee. Canadian Cardiovascular Society Atrial Fibrillation Guidelines 2010: prevention and treatment of atrial fibrillation following cardiac surgery. Can J Cardiol. 2011;27:91-97
- Pagana KD, Pagana TJ eds. Mosby’s Diagnostic and Laboratory Test Reference. 9th ed. St. Louis: Elsevier-Mosby; 2009
- Skidmore-Roth L. ed. Mosby’s drug guide for nurses. 9th ed. St. Louis: Elsevier-Mosby; 2011
- Skidmore-Roth L, ed. Mosby’s nursing drug reference. 24th ed. St. Louis: Elsevier-Mosby; 2011
- Stiell IG, Macle L CCS Atrial Fibrillation Guidelines Committee. Canadian Cardiovascular Society Atrial Fibrillation Guidelines 2010: management of recent-onset atrial fibrillation and flutter in the emergency department. Can J Cardiol. 2011;27:38-46
- Skanes AC, Healey JS, Cairns JA. Focused 2012 Update of the Canadian Cardiovascular Society Atrial Fibrillation Guidelines: Recommendations for Stroke Prevention and Rate/Rhythm Control. Can J Cardiol 2012; 28: 125-136
Journals/Clinical Trials:
- e-Therapeutics
- Lexicomp
- RxList
- Epocrates
- Thrombosis Canada
Journals/Clinical Trials:
- Connolly SJ, Camm A.J, Halperin JL, et al. Dronedarone in High-Risk Permanent Atrial Fibrillation (PALLAS). N Engl J Med 2011; 365:2268-76
- Connolly SJ, Eikelboom J, Joyner C, et al. Apixaban in Patients with Atrial Fibrillation. N Engl J Med 2011; 364:806-17
- Genest J, McPherson R, Frohlich J, et al. 2009 Canadian Cardiovascular Society/Canadian guidelines for the diagnosis and treatment of dyslipidemia and prevention of cardiovascular disease in the adult – 2009 recommendations. Can J Cardiol 2009; 25: 567-579
- Giugliano RP, Ruf CT., Braunwald E, et al. Edoxaban versus warfarin in patients with atrial fibrillation. N Engl J Med 2013;369:2093-2104
- Gladstone DJ, Spring M, Dorian P et al. Atrial Fibrillation in Patients with Cryptogenic Stroke. N Engl J Med 2014;370:2467-77
- Granger CB, Alexander JH, McMurray JJV, et al. Apixaban versus Warfarin in Patients with Atrial Fibrillation. N Engl J Med 2011; 365:981-92
- MominJH, Hughes GJ. Andexanet Alfa (Andexxa®) for the Reversal of Direct Oral Anticoagulants Pharmacy and therapeutics 2019 Sep; 44: 530-532
- Okin PM, Wachtell K, Kjeldsen SE, et al.Incidence of atrial fibrillation in relation to changing heart rate over time in hypertensive patients: the LIFE study. Circ Arrhythm Electrophysiol. 2008; 1:337-43
- Patel MR, Mahaffey KW, Garg J, et al. Rivaroxaban versus Warfarin in Nonvalvular Atrial Fibrillation. N Engl J Med. 2011; 365:883-91
- Pollack CV Jr, Reilly PA, van Ryn J. Idarucizumab for Dabigatran Reversal – Full Cohort Analysis. N Engl J Med. 2017;377:431-441. DOI: 10.1056/NEJMoa1707278
- Roy D, Talajic M, Dorian P, et al for the Canadian Trial of Atrial Fibrillation Investigators, Amiodarone to Prevent Recurrence of Atrial Fibrillation. N Engl J Med 2000; 342:913-920
- Siegal DM, Curnutte JT, M.D. Connolly SJ, Andexanet Alfa for the Reversal of Factor Xa Inhibitor Activity. N Engl J Med 2015; 373:2413-2424. DOI: 10.1056/NEJMoa1510991
- The ACTIVE Writing Group on behalf of the ACTIVE Investigators. Clopidogrel plus aspirin versus oral anticoagulation for atrial fibrillation in the Atrial fibrillation Clopidogrel Trial with Irbesartan for prevention of Vascular Events (ACTIVE W).The Lancet. 2006: 367: 1903-1912