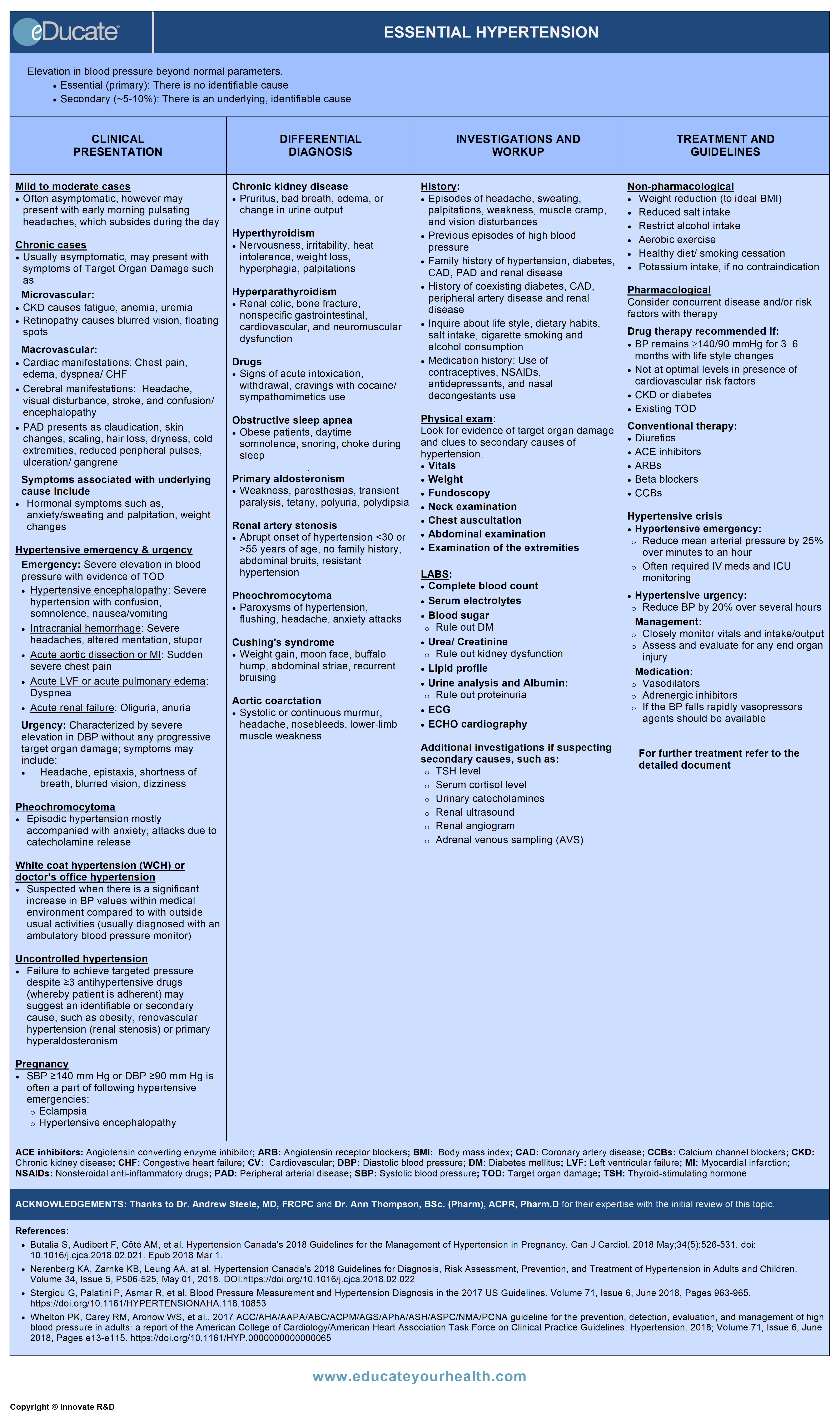
Essential Hypertension
ACKNOWLEDGEMENTS:
Thanks to Dr. Andrew Steele, MD, FRCPC, Medical Director and Chief of Nephrology, Lakeridge Health, Associate Professor of Medicine (Adjunct) Queens University, ON Canada, and Dr. Ann Thompson, BSc. (Pharm), ACPR, Pharm.D, Medical Director and Chief of Nephrology, Lakeridge Health, Associate Professor of Medicine (Adjunct) Queens University, ON Canada for their expertise with the initial review of this topic.
[pdf-embedder url=”https://www.educateyourhealth.com/wp-content/uploads/2019/03/Hypertension-Brochure.pdf” width=”750″]
Definition
Elevation in blood pressure beyond normal parameters
- Essential (Primary) – No identifiable cause
- Secondary (~5-10%) – Identifiable underlying cause


BP measurement methods:
- Automated office blood pressure (AOBP) preferred method of performing in-office BP measurement
- a displayed mean SBP ≥135 mm Hg or DBP ≥85 mm Hg is high
- Office blood pressure measurement (OBPM)
- Oscillometric (electronic) – preferred method
- Auscultatory (mercury, aneroid)
- When using mean OBPM, a SBP ≥140 mm Hg or a DBP ≥90 mm Hg is high, and an SBP between 130-139 mm Hg and/or a DBP between 85 and 89 mm Hg is high-normal
- Ambulatory blood pressure measurement (ABPM)
- patients can be diagnosed as hypertensive if the mean awake SBP is ≥135 mm Hg or the DBP is ≥85 mm Hg or if the mean 24-hour SBP is ≥130 mm Hg or the DBP is ≥80 mm Hg
- Home blood pressure measurement (HBPM)
- Patients can be diagnosed as hypertensive if the mean SBP is ≥135 mm Hg or the DBP is ≥85 mm Hg
Etiology
Primary (essential hypertension)
- No identifiable cause
Secondary
- Endocrine (e.g. hyperaldosteronism, thyroid, parathyroid, pheochromocytoma)
- Renal disorders (e.g. glomerulonephritis)
- Obstructive sleep apnea
- Metabolic syndrome
- Coarctation of aorta
- Drug-induced
- Genetic (rare)
- Lifestyle
- Others
Risk factors
- Cigarette smoking
- Age (men >55, women >65)
- Obesity (body mass index ≥30 kg/m2)
- Dyslipidemia
- Diabetes mellitus and metabolic syndrome
- Physical inactivity
- Diet-high sodium intake
- Family history of premature vascular disease
Epidemiology
- Third leading cause of death worldwide
- Increases with age
- An estimated 1.13 billion people worldwide have hypertension
- Nearly 108 million (45%) of adults in the United States have hypertension
- About 1 in 5 adults or ~7.5 million people in Canada live with hypertension
- Affects 25% of the adult Canadian population
- Typical onset between 25 and 55 years
Pathophysiology
Though still poorly understood, various factors have been suggested including enhanced beta-adrenergic response, increased angiotensin II activity, and excess mineralocorticoids, which ultimately lead to:
- Increased peripheral vascular resistance
- Increased cardiac output
- Increased blood volume
Genetic factors account for 30% of cases (patients with family history of one or both parents).
Clinical Presentation
1) Mild to moderate cases:
- Often asymptomatic
- May present with early morning pulsating headaches, which subsides during the day
2) Chronic cases:
– Usually asymptomatic
– May present with
Symptoms of target organ damage (TOD) including
Microvascular:
- Chronic kidney disease (CKD)
- Fatigue
- Anemia
- Signs and symptoms of uremia
- Labs: Proteinuria, reduced GFR
- Retinopathy
- Blurred vision
- Floating spots
- Loss of vision
Macrovascular damage:
- Cardiac manifestations
- Chest pain
- Edema
- Dyspnea/ CHF
- Cerebral manifestations
- Headache
- visual disturbance
- Stroke
- Confusion/ encephalopathy
- Peripheral arterial damage
- Claudication
- Skin changes, dryness, scaling, hair loss
- Cold extremities
- Reduced peripheral pulses
- Ulceration, gangrene
– Associated with underlying cause include
- Edema due to chronic kidney disease
- Hormonal symptoms such as weight changes, sweating, tachycardia, anxiety
3) Hypertensive Emergency and Urgency:
Emergency:
Characterized by a severe elevation in blood pressure with evidence of target organ damage (TOD). CHEP 2012 guidelines suggest a DBP of ≥130 with TOD, while JNC VII suggests BP of >180/120 mmHg complicated by evidence of impending or progressive target organ dysfunction.
- Hypertensive encephalopathy: Accelerated hypertension associated with somnolence, confusion, visual disturbances, nausea and vomiting
- Intracranial hemorrhage: Sudden severe headache followed by altered mentation, paralysis, stupor, and coma
- Acute aortic dissection or MI: Sudden severe pain in the chest
- Acute left ventricular failure or acute pulmonary edema: Dyspnea, edema
- Acute renal failure: Oliguria, anuria, altered mentation
Urgency:
Characterized by severe elevation in BP (>180 systolic ± >120 diastolic) without any progressive target organ damage, i.e. patient may be symptomatic but no TOD)
- Blurred vision, headache, dizziness, edema, nausea
- Epistaxis
- Shortness of breath
4) Pheochromocytoma:
Episodic hypertension mostly accompanied with anxiety attacks due to catecholamine release
- Palpitation
- Perspiration
- Pallor
- Tremor
- Vomiting
- Angina
- Orthostatic hypotension
5) White coat hypertension, WCH (doctors office hypertension)
- Is suspected when there is a significant increase in BP values within the medical environment compared to with outside usual activities (usually diagnosed with an ambulatory blood pressure monitor)
- Once diagnosed, accurate home BP values may be the best guide for therapy
6) Uncontrolled hypertension:
Failure to achieve targeted pressure despite ≥3 antihypertensive drugs (whereby patient is adherent) may suggest an identifiable or secondary cause, such as obesity, renovascular hypertension (renal stenosis) or primary hyperaldosteronism.
7) Pregnancy:
- Hypertension in pregnancy is defined as an SBP 140 mm Hg and/or a DBP 90 mm Hg (average of at least 2 measurements taken at least 15 minutes apart)
- BP levels between 140/90 mm Hg and < 160/110 mm Hg are considered non-severe hypertension in pregnancy
- A systolic BP ≥160 mmHg or a diastolic BP ≥110 mmHg is often a part of following hypertensive emergency presentation:
- Eclampsia: Icteric, pruritus, headaches, seizures
- Hypertensive encephalopathy: Restlessness, irritability, headaches, seizure, and coma
Differential Diagnosis
Differential diagnosis of secondary hypertension is intimately linked to the etiology and includes:
Chronic kidney disease (assess creatinine, eGFR, proteinuria)
- Pruritus, bad breath, edema, change in urine output
Hyperthyroidism
- Nervousness, irritability, heat intolerance, weight loss, hyperphagia, palpitations
Hyperparathyroidism (assess serum calcium)
- Renal colic, bone fracture, nonspecific gastrointestinal, cardiovascular, and neuromuscular dysfunction
Drugs (prescription, over-the-counter, herbal supplements, illicit drugs)
- Signs of acute intoxication, withdrawal, cravings with cocaine/sympathomimetics use
Obstructive sleep apnea
- Obese patients, daytime somnolence, snoring, choking during sleep.
Primary aldosteronism
Consider when i) K+ <3.5 mmol/L, ii) K+ <3.0 mmol/L on diuretic, iii) Resistant hypertension
- Presents with weakness, paresthesias, transient paralysis, tetany, polyuria, polydipsia
Renal artery stenosis
Consider if resistant hypertension and low serum potassium.
- Presents with abrupt onset of hypertension <30 or >55 years of age, no family history, abdominal bruits, resistant hypertension, acceleration of previously well-controlled hypertension
Pheochromocytoma
- Paroxysms of hypertension, flushing, headache, anxiety attacks
Cushing’s syndrome
- Weight gain, moon face, buffalo hump, abdominal striae, recurrent bruising
Aortic coarctation
- Systolic or continuous murmur, headache, nosebleeds, lower-limb muscle weakness
Investigation and Workup
HISTORY:
- Episodes of headache, sweating, palpitations, weakness, muscle cramp, and vision disturbances
- Previous episodes of high blood pressure
- History of diabetes, CAD, peripheral artery disease and renal disease
- History of coexisting diseases such as migraine, gout, asthma, heart failure and BPH
- Inquire about sedentary lifestyle, dietary habits, salt intake, cigarette smoking and alcohol consumption
- Family history of hypertension, diabetes, CAD, peripheral artery disease and renal disease
- Medication history
- Oral contraceptives
- NSAIDs
- Antidepressants
- Nasal decongestants
PHYSICAL EXAM:
Look for evidence of target organ damage and clues to secondary causes of hypertension.
– Vitals:
- Confirm BP and consider an automated BP cuff e.g. The BP Tru™
– General appearance:
- Example, Cushingoid facies
– Weight:
- Assess for obesity, metabolic syndrome
– Fundoscopy:
- Papilledema
- Hypertensive retinopathy
– Neck exam:
- Carotid bruits
- Distended veins
- Enlarged thyroid gland
– Chest auscultation for
- Abnormal heart sound
- Pulmonary edema
– Abdominal exam:
- Renal bruits
- Palpable kidney
- Masses
- Abnormal aortic pulsations
– Examination of the extremities:
- Diminished/ absent peripheral arterial pulsations
- Bruits
- Edema
LABS:
- Complete blood count (CBC)
- Serum electrolytes
- Uric acid
- Blood sugar: Fasting blood glucose and/or glycated hemoglobin (A1C)
- Creatinine and eGFR
- Lipid profile: Fasting or non-fasting
- Urine analysis and albuminuria assessment with urine albumin/creatinine ratio (ACR)
- Electrocardiogram (ECG)
Additional investigations for secondary causes:
- Plasma renin level (renovascular hypertension)
- Serum aldosterone or 24-hour urine aldosterone
- 24-hour urinary free cortisol level
- Thyroid-stimulating hormone (TSH) level
- Urinary catecholamines and fractionated metanephrines
- Adrenal venous sampling (AVS): In patients with primary hyperaldosteronism and a definite adrenal mass considering surgery
IMAGING
- Chest X-ray
- Renal ultrasound
- Renal angiogram (usually with CT/CTA or MRI/MRA)
- CT scan of abdomen
- ECHO cardiography
Treatment

NON-PHARMACOLOGICAL THERAPY
– Weight:
Aim for an ideal Body Mass Index, decrease as little as 4.5 kg in weight significantly reduces BP.
Target: BMI = 18.5 to 24.9 kg/m2
Formula: BMI = weight in kilograms / height in meter 2
– Waist circumference:

– Salt intake:
To decrease BP, consider reducing sodium intake toward 2000 mg (5 g of salt or 87 mmol of sodium) per day.

1,500 mg sodium (Na) = 65 mmol sodium (Na) = 3.75 g of salt (NaCl) = 1/2 level teaspoon of table salt
– Alcohol: Restrict intake to a maximum of
- Two standard drinks per day or 14 drinks per week for men and 9 drinks per week for women
One standard drink is equivalent to:
- 5 oz./142 ml of wine (12% alcohol)
- 1.5 oz./43 ml of spirits (40% alcohol)
- 12 oz./341 ml regular strength beer (5% alcohol)
– Potassium intake:
In patients not at risk of hyperkalemia, increase dietary potassium intake to reduce BP
When appropriate, patients with hypertension should be encouraged to consume foods with higher potassium content (e.g. fresh fruits, vegetables, and legumes)
– Exercise:
Moderate intensity dynamic exercise, such as brisk walking for 30-60 minutes, 4-7 days per week in addition to the routine activities of daily living
– Diet:
A diet rich in fruits, vegetables, and dairy products with reduced saturated and total fat can substantially lower BP – consider the DASH diet.
– Smoking:
Cessation of smoking and smoke-free environment is important to reduce hypertension, stroke, and cardiovascular risk.
PHARMACOLOGICAL THERAPY
Indications:
- Average SBP >160 or DBP >100 mm Hg without TOD or risk factors
- Average SBP ≥140 and/or DBP ≥90 mm Hg for patients with target organ damage e.g. left ventricular hypertrophy
- Diabetes or chronic kidney disease with BP ≥130/80 mm Hg
- Chronic kidney disease with BP ≥140/90 mm Hg
- Presence of other risk factors (over 90% of Canadians with hypertension have other risk factors)
Treatment Gap Alert: Many younger hypertensive Canadians with multiple cardiovascular risks are currently not treated with pharmacotherapy. Health care professionals need to be aware of this important care gap and recommend pharmacotherapy.
Considerations in the selection of therapy:
- Race: Diuretics preferred over renin-angiotensin system (RAS) inhibitors for African-Americans
- Age
- Coexisting diseases and therapies
- Quality of life (QOL)
- Economic consideration
- Dose per day (compliance factor)
– Diuretics:
- Thiazides are used as 1st line agents because of effectiveness, compliance, and cost
- Loop diuretics should be used in patients with decreased renal function, defined as CrCl <20-30 mL/min
- Aldosterone antagonists: Prescribed in patients with primary hyperaldosteronism or those with resistant hypertension
– Βeta blockers:
- May be used 1st line for patients with ischemic heart disease, CHF, those with migraine
- Not indicated 1st line in patients over the age of 60 years
– ACE inhibitors:
- Should be considered in patients with diabetes, chronic kidney disease, atrial fibrillation, CAD or CHF
- Contraindicated in pregnancy
– Angiotensin receptor blocking agents:
- Considered in patients with diabetes, renal insufficiency, chronic kidney disease, or CHF (when ACE intolerant)
- Contraindicated in pregnancy
– Dihydropyridine calcium channel blockers:
- Considered in patients with isolated systolic hypertension, angina, and those at high CV risk
- Shown to be safe in pregnancy
– Non-dihydropyridine calcium channel blockers:
- Considered in patients with atrial arrhythmia, tachycardia, stable angina, concomitant migraine
– Alpha-adrenoceptor antagonists:
- Non-selective antagonists are usually reserved for use in hypertensive emergencies caused by a pheochromocytoma or as 4th line agents
- Consider in hypertensive males with BPH
– Direct renin inhibitors:
- Indicated for the treatment of mild to moderate essential hypertension and reduction of proteinuria in addition to ACEIs or ARBs
- Contraindicated in pregnancy
– Drugs with central sympatholytic action (alpha agonists, central):
- Effective in hypertensive patients with renal disease because they do not compromise renal function; considered as 4th line agents
- Methyldopa is traditionally considered as first-line therapy in pregnancy
– Vasodilators:
- Usually prescribed as adjunct therapy with other BP drugs and rarely are used alone
- Hydralazine also may be used to control high BP in pregnant women
- Nitroglycerin/ nitroprusside can be used in hypertensive emergencies
– Combination drugs:
May be used to:
- Simplify regimen and improve adherence
- Avoid side effects that may occur from high doses of a single agent
- If the BP is >20 mm Hg systolic ± >10 mm Hg diastolic above target – consideration should be given initially to start with 2 drugs from different classes, preferably as a combination product with the exception of beta-blockers with non-DHP-CCBs and ACEI with ARBs
If hypertension is NOT adequately controlled with a single agent, the patient should follow up monthly or more frequently if severe hypertension. Also, consider
- Patient non-adherence: Cost and adverse effects/allergy should be considered
- Suboptimal dose: Increase dose if the patient is considered adherent, however combination therapy is usually preferred to maximal doses of single agents
- If no change in BP and the patient is adherent, 1st choice option may be ineffective and a new agent should be substituted
- Add in a second drug from another class; to improve control, and minimize adverse effects caused by the maximum dose of single agents
Specific Paradigms for Treatment of Hypertension:
- Isolated hypertension (Non-DM)
- Diabetes with hypertension
- Cardiovascular disease with Hypertension
- Stroke and TIA with hypertension
- Non-DM chronic kidney disease with hypertension
- PAD with hypertension
- Dyslipidemia with hypertension
HYPERTENSIVE EMERGENCY AND URGENCY:
Emergency:
- Initially reduce mean arterial BP by no more than 25% within minutes to an hour, once stable, further stabilization to 160/100-110 mm Hg within the next 2-6 hours to avoid further organ damage
Urgency:
- Avoid precipitous drop in BP. Aggressive dosing with intravenous drugs or even oral agents, to rapidly lower BP is not without risk
- Patients with stage II hypertension with associated symptoms such as severe headache, shortness of breath, epistaxis, or severe anxiety, should have their BP lowered up to 20% over several hours
- Some hypertensive urgencies may benefit from treatment with oral, short-acting agents. Most importantly, patients should not leave the ER without a confirmed follow-up appointment within a few days
Management:
- Monitor for end-organ injury:
- Abnormal neurologic signs (stroke, seizures)
- Severe headache
- Pulmonary edema
- Chest pain (MI, aortic dissection)
- Vision difficulty (retinal edema, hemorrhage)
- Hospitalization, IV treatment, and ICU monitoring usually required for hypertension emergency/urgency
- Parenteral antihypertensive agents may include:
- Vasodilators: e.g. Sodium nitroprusside, nitroglycerin, hydralazine
- Adrenergic inhibitors: e.g. Labetalol, methyldopa, phentolamine
- ACEIs: e.g. Enalaprilat
- Diuretics may be used to induce diuresis if required
- Ionotropic pressure support may be required for precipitous drop in BP
Special Considerations:
Hypertension and stroke
- Avoid overzealous BP lowering in acute stroke. Treat extreme BP elevation (systolic >220 mmHg, diastolic >120 mm Hg) by 15-25% over the first 24 hours with gradual reduction thereafter
- If eligible for thrombolytic therapy in acute stroke, treat very high BP (>185/110 mm Hg)
- In secondary prevention, the benefits of BP lowering is seen in both normotensive and hypertensive patients
- ACEI plus diuretic or ARB – based treatment should be considered
Aortic dissection
- Emergent cases, often requiring surgical management, especially in ascending aortic dissection
- Do not use sodium nitroprusside without beta-blockers, (increases the chances of aortic rupture)
Pheochromocytoma
- Alpha and beta-adrenergic receptors are stimulated by excess catecholamine in pheochromocytoma
- Preferred treatment is surgical resection of tumor, following α-adrenergic blockade to avoid catecholamine surge
- β-Adrenergic blockade alone may result in more severe hypertension owing to the unopposed α-adrenergic stimulation
Elderly hypertensive patient (age >60 years)
- May also have coexisting medical conditions
- Dosage should be increased gradually
- Diuretics, CCBs and ACE inhibitors/ARBs are good choices
- Avoid excess BP lowering especially if postural hypotension
Hypertension in patients of African descent
- Beta blockers and ACE inhibitors are less effective
- Calcium channel blockers, diuretics and possibly ARBs are the good choice
Obese hypertensive patient
- Weight reduction is the mainstay of non-pharmacological therapy
- Treatment is similar to isolated hypertension. However, there may be an associated risk of left ventricular hypertrophy, endothelial dysfunction, renal hyperfiltration, microalbuminuria, hence ACEI or ARB may be a reasonable option
The diabetic patient
- Usually require combination therapy to achieve desired levels ≤130/80 mm Hg
- Should start with ACE inhibitors or ARBs, and consider combination therapy if BP is >20 mm Hg systolic ± >10 mm Hg diastolic above target
- Caution with blockers because of their masking hypoglycemic symptoms
Patient with chronic kidney disease
- Most patients with hypertension require combination therapy to achieve optimal BP goals <130/80 mm Hg
- Initially start with diuretics (especially loop diuretics if Clcr <20-30 mL/min) and ACEI or ARBs
Patient with left ventricular hypertrophy (LVH)
- May start with ACEI or ARBs. Long-acting CCB or thiazide diuretics are other options
Patients with coronary artery disease (CAD)
- Increased risk of unstable angina (UA) and myocardial infarction (MI)
- May start with beta-adrenergic antagonist, long-acting CCB or ACE inhibitors
- Cautiously use non-dihydropyridine calcium channel blockers in MI and cardiac conduction system disease
Patients with heart failure (HF)
- ACEI and Beta blocker (ARB if ACEI intolerant)
- Titrate doses of beta-blockers and ACEI/ ARB to those used in clinical trials
- Avoid calcium channel blockers because of negative inotropic effects
- Add aldosterone antagonist in class 2, 3 or 4 HF
Pregnancy and hypertension
- Treatment is recommended for average SBP 140 mm Hg or DBP 90 mm Hg in pregnant women with chronic hypertension, gestational hypertension, or preeclampsia
- Pregnant women receiving antihypertensive therapy with chronic hypertension or gestational hypertension or preeclampsia, a DBP of 85 mm Hg should be targeted
- Avoid non-pharmacologic therapy such as:
- Weight reduction
- Exercise
- Oral alpha methyldopa has the largest amount of safety data and is still preferred
- First-line monotherapy drugs to be considered are labetalol, long-acting oral nifedipine, or other oral b-blockers (acebutolol, metoprolol, pindolol, and propranolol)
- Second-line drugs to be considered are clonidine, hydralazine, and thiazide diuretics
- Alpha-methyldopa has the largest amount of safety data and is still preferred
- ACEIs, ARBs, and nitroprusside are contraindicated in the pregnancy
Surgical/ Interventional
Treatment of renovascular hypertension
- Percutaneous transluminal angioplasty
- Stent placement (for fibromuscular hyperplasia and for discrete stenotic arteriosclerotic lesions not involving the renal artery ostium)
- Rarely bypass graft
[/cq_vc_tab_item][cq_vc_tab_item tabtitle=”Medication Dose”]MEDICATIONS
Diuretics
- Thiazide diuretics
- Loop diuretics
- Aldosterone receptor blockers
- Inhibitors of renal epithelial Na+ channels
Mechanism:
- Block Na/Cl transport in the proximal part of renal distal convoluted tubules
Dose:
Hydrochlorothiazide
- Initial 12.5 mg PO daily. Usual dose 25 mg PO daily; minimal benefit for lowering BP beyond 25 mg, however, side effects (such as hypokalemia and hyponatremia) increase
Chlorthalidone
- Initial 12.5 mg PO daily, increase to 25 mg/day if needed. Maximum dose is 50 mg/day, although there is minimal additional BP lowering effect beyond 25 mg/day
Indapamide
- Initial 1.25 mg PO daily; usual 2.5 mg/day, can be used when renal function <30 mL/min
- Titration: Increase by 1.25 mg PO every 4 weeks, according to blood pressure response; Max. 2.5 mg daily
Mechanism:
- Loop Diuretics → Block Na/K/Cl transporter in the renal loop of Henle
Dose:
Furosemide
- Initial 20 mg PO BID, it can be given 40 mg PO BID and then adjusted according to the response
Note: Will only consider if eGFR <30 mL/minute
Mechanism:
- Blocks aldosterone receptors in renal collecting tubule → results in increased excretion of sodium and water and decreased excretion of potassium
Dose:
Spironolactone
- Initial 25-100 mg PO in single or divided doses, should be continued for 2 weeks then adjustments should be made according to the response
Eplerenone
- Initial 50 mg PO Daily for should be continued for 4 weeks, can go up to 50 mg PO BID. No therapeutic benefits observed with >100 mg/day
Inhibitors of renal Epithelial Na+ Channels
Mechanism:
- Disrupts sodium ↔ potassium exchange in the distal convoluted tubule and collecting ducts of the nephron
- Inhibits Sodium-Potassium-ATPase
- Decreases calcium excretion
- Increases magnesium loss
Dose:
Amiloride
- Initial 5 mg PO daily, usual 5-10 mg PO daily; Max. 20 mg/day (usually used in combination with another antihypertensive)
Triamterene
- Initial 50 mg PO daily; usual 50-100 mg PO daily (usually used in combination with thiazide diuretic)
Beta-adrenergic blocking agents
Cardioselective:
- Acebutolol
- Atenolol
- Bisoprolol
- Metoprolol
- Nebivolol
Non- Cardioselective:
- Carvedilol
- Nadolol
- Propranolol
- Timolol
- Pindolol
- Labetalol
Mechanism:
- Block beta receptors
- Decrease heart rate and cardiac output
- Decrease renin release
Dose:
Cardioselective:
Acebutolol
- Mild to moderate hypertension 200-400 mg PO daily in 2 divided doses
- Patient with severe hypertension may respond to higher doses
Atenolol
- Initial 25-50 mg PO daily, doses >100 mg/day show no additional benefit
Bisoprolol
- In some case initial 2.5 mg PO daily is preferable (especially in renal and hepatic impairment), usual 5 mg PO daily; may increase up to 20 mg/day if required
Metoprolol
Conventional tablets:
- Initial 25-50 mg/day PO BID; usual 100-200 mg/day in divided doses; Max. 400 mg/day in 2 divided doses
Extended-release tablets:
- Initial 25-100 mg PO daily; usual 100-200 mg PO daily
IV Metoprolol:
May be used to control hypertension/ventricular rate control in patients NPO or nonfunctioning GI tract.
- Initial low dose of 1.25-5 mg IV every 6-12 hrs
Nebivolol
- Initial 5 mg PO once daily, usual 5 to 10 mg once daily; can be increased at two-week intervals up to 20 mg once daily
Non- Cardioselective:
Carvedilol
Extended-release capsules:
- Initial 10 mg PO daily; Max. 80 mg/day
Immediate-release tablets (not indicated in Canada for HTN):
- Initial 6.25 mg PO BID; usual 12.5-25 mg PO BID; Max. 25 mg PO BID
Labetalol
- Initial 100 mg PO BID; usual 200-400 mg PO BID
- In severe hypertension maximum dose 1200 mg/day
- Titration: Increase dosage by 100 mg PO BID every 2-3 days
Hypertensive emergency
- IV: Initial 10-20 mg IV over 2 min x 1
- Additional doses of up to 40-80 mg at 10-minute intervals may be required to achieve desired BP. Total cumulative dose of 300 mg; Max. 300 mg/day IV
- IV infusion: Initial 0.5-2 mg/minute continuous IV infusion (discontinue after 2.5 hrs of infusion)
- Oral dose following IV: Initial 100 mg PO daily; maintenance dose 200-400 mg PO in 2 divided doses
Nadolol
- Initial 40 mg PO daily; usual 40-80 mg PO daily; Max. 320 mg/day
- Titration: Gradually increase by 40-80 mg/day every 3-7 days
- In renal impairment depending on the CrCl dose interval is increased and doses are reduced
Propranolol
Conventional tablets:
- Not indicated for hypertension
Long acting (extended- release) capsules:
- Initial 80 mg PO; usual 160-320 mg PO daily; Max. 320 mg/day
- Titration: Increase dose 120-160 mg/day every 3-7 days
Timolol
- Initial 10 mg PO BID; usual 20-40 mg/day in 2 divided doses; Max. 60 mg/day
- Titration: May increase dose gradually at 5 mg BID intervals every 14 days
Pindolol
- Initial 5 mg PO twice daily; usual dose is 10-40 mg PO BID; Max. 60 mg/day
- Titration: Increase gradually by 10 mg/day every 3-4 wks
ACE (angiotensin-converting enzyme) inhibitors
- Benazepril
- Captopril
- Cilazapril
- Enalapril
- Fosinopril
- Lisinopril
- Perindopril
- Ramipril
- Quinapril
- Trandolapril
Mechanisms:
- Inhibition of the renin-angiotensin-aldosterone system
- Inhibit bradykinin degradation
- Stimulate vasodilating prostaglandin synthesis
- Reduce sympathetic nervous system activity
Caveat: Inhibitors of the RAS (ACEI/ARB/DRI) might precipitate acute renal failure in the setting of conditions/illnesses that can be associated with dehydration.
Dose:
Benazepril
- Initial: 1 mg once daily. Usual: 20 mg once daily; Maximum: 40 mg daily
Captopril
- Initial 12.5-25 mg PO BID or TID; usual 50 mg PO BID or TID; Max. 450 mg/day
- Titration: Increase by 12.5-25 mg/dose every 1-2 week; up to 50 mg 3 times/day
- Usually after 50 mg PO TID, consider adding a diuretic (thiazide)
Cilazapril
- Initial 2.5 mg PO once daily. Usual: 2.5 to 5 mg once daily; Maximum: 10 mg daily
- Elderly: Initial 1.25 mg PO once dailyRenal Impairment: Creatinine Clearance
- > 40 mL/min: 1 mg once daily; Max. 5 mg once daily
- 10 – 40 mL/min: 0.5 mg once daily; Max. 2.5 mg once daily
- < 10 mL/min: 0.25 – 0.5 mg once or twice a week
Hepatic Impairment:
Cirrhosis: Initial ≤ 0.5 mg PO once daily
Enalapril
- Initial 2.5-5 mg PO daily; usual 2.5-40 mg/day in 1-2 divided doses; Max: 40 mg/day
Enalaprilat IV
- Initial 1.25 mg IV over 5 minutes every 6 hrs; usual 0.625-1.25 mg IV over 5 minutes given every 6 hrs, up to 36 hrs
- If concomitant diuretic use – begin with 0.625 mg IV over 5 minutes
Fosinopril
- Initial: 10 mg PO once daily. Usual: 20 mg daily as a single dose; Maximum: 40 mg daily
Lisinopril
- Start 10 mg PO daily; usual 10-40 mg PO daily; Max. 80 mg/day
- If concomitant diuretic – use cautiously, begin with 5 mg PO daily
- Moderate renal failure (CrCl 10-30): Begin with 5 mg PO daily; only if the decline/failure is not secondary to bilateral renal stenosis
- Dialysis patients: Begin with 2.5 mg once daily (adjust according to BP response)
Perindopril
- Initial 2-4 mg PO daily; usual 4-8 mg PO daily; Max. 16 mg/day
Ramipril
- Initial 2.5 mg PO daily (Max. 20 mg/day). Adjust at 1-2 week intervals by doubling dose, or 5 mg increments
Quinapril
- Initial: 10 mg once daily. Usual: 10 to 20 mg once daily; Maximum: 40 mg daily
Trandolapril
- Initial 1 mg PO daily or 2 mg PO daily in black patients; usual 2-4 mg PO daily. Adjust dosage at weekly intervals
Angiotensin receptor blocking agents
- Azilsartan
- Candesartan
- Eprosartan
- Telmisartan
- Irbesartan
- Losartan
- Olmesartan
- Valsartan
Mechanisms:
- Block AT1 angiotensin receptors
- Blocks the vasoconstrictor and aldosterone secreting effects of angiotensin II
- Reduce vasoconstriction
Caveat: Inhibitors of the RAS (ACEI/ARB/DRI) might precipitate acute renal failure in the setting of conditions/illnesses that can be associated with dehydration.
Dose:
Azilsartan
- Initial 40 mg PO once daily. Max. 80 mg once daily
Candesartan
- Initial 8-16 mg PO daily; Max. 32 mg/day
Eprosartan
- Initial 400-600 mg PO daily. Total daily dose 400-800 mg/day in 1-2 divided doses; Max 800 mg daily
Irbesartan
- Initial 150 mg PO daily; usual 150-300 mg PO daily; Max. 300 mg/day
Note: Starting dose in volume-depleted patients should be 75 mg.
Losartan
- Initial 50 mg PO daily; usual 25-100 mg PO daily in 2 divided doses; Max. 100 mg
Telmisartan
- Initial 40 mg PO daily; usual 20-80 mg PO daily; Max. 80 mg/day
Olmesartan
- Initial: 20 mg once daily. Usual: 20 to 40 mg once daily; Maximum: 40 mg daily and 29 mg in mild to moderate renal impairment
Valsartan
- Initial 80-160 mg PO daily, in non-volume depleted patients; Max. dose is 320 mg PO daily
- Aliskiren
Mechanism:
Decrease plasma renin activity → inhibits conversion of angiotensinogen to angiotensin I → results in decreased the formation of angiotensin II
Caveat: Inhibitors of the RAS (ACEI/ARB/DRI) might precipitate acute renal failure in the setting of conditions/illnesses that can be associated with dehydration.
Dose:
Aliskiren
- Initial 150 mg PO daily; Max. 300 mg/day
Calcium channel blocking agents (CCBs)
Non- Dihydropyridines:
- Diltiazem
- Verapamil
Dihydropyridines:
- Amlodipine
- Felodipine
- Nifedipine
Mechanisms:
- Blocks the inward movement of calcium by binding to the L-type calcium channels in the heart and in smooth muscle of the peripheral vasculature
- This decreases intracellular calcium leading to a reduction in muscle contraction
- Significant reduction in afterload but not preload
Dose:
Non- Dihydropyridines:
Diltiazem
- Initial 120-240 mg Po daily, usual 180-360 mg PO in 2 divided doses, Max. 360 mg/day
- Titration: Over 7-14 days
Canadian extended-release formulations
- XC or CD: Initial 120-240 mg PO daily; usual 240-360 mg PO daily
USA extended-release formulations-XR form and LA
- XR: Initial 180-240 mg PO daily; usual 180-480 mg PO daily
- LA: Initial 180-240 mg PO daily; usual 120-540 mg PO daily
Verapamil
Immediate-release form:
- Initial 80 mg TID or, usual 80 mg PO TID; Max. 480 mg/day; Elderly: Initial 40 mg PO TID
Verapamil (SR):
- Initial 180 mg every morning, usual 120-480 mg/day; Max. 480 mg/day; Elderly: Initial 120 mg every morning
Extended-release form (PM):
- Initial 200 mg at night, usual 200 mg at bedtime; Max. 400 mg/day; Elderly: Initial 100 mg at bedtime
Verapamil (HS):
- Initial 180 mg PO at bedtime; usual 240-480 mg PO at bedtime; Max. 480 mg PO at bedtime
Dihydropyridines:
Amlodipine
- Initial 5 mg PO daily or 2.5 mg PO daily in elderly; usual 5-10 mg PO once daily; Max. 10 mg/day
- Titration: Increase 2.5 mg over 1-2 wk (up to a maximum dose)
Felodipine
- Initial 2.5-5 mg PO daily; usual 5-10 mg PO daily; Max. 20 mg/day
Nifedipine – DO NOT USE immediate release formulation
Extended-release:
- Initial 30-60 mg PO daily; usual 30-90 mg PO daily; Max. 120 mg/day
- Titration: Increase dose by every 7-14 days
Nicardipine
- Oral: Initial 20 mg PO TID; usual 20-40 mg PO TID; Max. 120 mg/day
– Other Dihydropyridine NOT available in Canada:
Alpha-adrenoceptor antagonists
Selective alpha-adrenoceptor antagonists
- Prazosin
- Terazosin
- Doxazosin
Non-selective alpha-adrenoceptor antagonists
- Phentolamine
Mechanism:
- Block postsynaptic alpha receptors
- Relax smooth muscle
- Lowers peripheral vascular resistance
Dose:
Prazosin
- Initial 2-3 mg PO TID daily; maintenance 2-20 mg in 2-3 divided doses; Max. 20 mg/day
Terazosin
- Initial 1 mg PO daily at bedtime; usual 1-10 mg daily at bedtime; Max. 20 mg/day
Doxazosin
- Initial 1 mg PO daily at bedtime; may increase dose to 2 mg daily, make subsequent adjustments by doubling dose at intervals of 2-4 weeks until desired effect is achieved; Max. 16 mg/day
- Note: Substantial risk of syncope/postural effects with dosages >4 mg/daily.
Phentolamine
Hypertensive crisis (especially secondary to catecholamine excess)
- IV: Initial 5-15 mg bolus
Agents with central sympatholytic action (alpha agonists, central)
- Clonidine
- Methyldopa
Mechanisms:
- Stimulates alpha-adrenergic receptors in the central nervous system → reduces efferent peripheral sympathetic outflow
Dose:
Clonidine
Oral:
- Initial 0.05 mg PO BID. Usual 0.1 mg/day PO daily
- Titration: May increase by 0.1 mg/day every week until desire response achieved, then taper dose gradually over 2-4 days
Transdermal (available in the US):
- Initial 0.1 mg/week; usual 0.1-0.3 mg/week
- Titration: May increase by 0.1 mg 1-2 week interval
Methyldopa
Oral:
- Initial 250 mg BID or TID; usual 250 mg to 1 g daily in 2-3 divided doses. Max. 3 g/day (divided) in adults; 1 g/day in elderly
- Titration: Adjust dosage every 2 days until an adequate response is achieved
Intravenous (IV):
- 250 mg to 1 g every 6-8 hr, maximum: 1 g every 6 hrs
- Hydralazine
- Minoxidil
- Nitroglycerin
- Nitroprusside
Mechanisms:
- Relax vascular smooth muscle
- Produce peripheral vasodilatation
- Decrease pre and after-load
- Reduces myocardial oxygen demand
- Nitroglycerin dilates coronary arteries
Dose:
Hydralazine
Oral:
- Initial 10 mg/day every 6 hrs for 2-4 days; usual 25 mg/day QID; Max. 300 mg/day
- Titration: Dosage may increase by 10-25 mg/dose every 2-5 days; up to a maximum dosage
Intravenous (maximum rate: 5 mg/minute):
- 10-20 mg every 4-6 hr
- Titration: May increase to 40 mg/dose
Intramuscular (IM):
- 10-50 mg every 4-6 hr
- Titration: May increase to 40 mg/dose
Minoxidil
- Oral: Initial 5-10 mg PO daily; usual 10-40 mg/day in 1-2 divided doses; Max. 100 mg/day
Nitroglycerin
In hypertensive emergency
- IV: 5 mcg/min; usual range 5-100 mcg/min; Max. 200 mcg/min
- Titration: Increase 5 mcg/minute every 3-5 min to 20 mcg/minute, if no response; increase 10-20 mcg/min every 3-5 min up to maximum dosage
Nitroprusside
In hypertensive emergency
- IV: Initial 0.25-0.3 mcg/kg/min; usual 3-4 mcg/kg/min; Max. 10 mcg/kg/min for 10 min
- Titration: Increase 0.5 mcg/kg/minute to maximum dosage till the desired effect achieved or adverse effect appears
COMBINATION DRUGS:
Examples of some commonly used agents
Diuretic combinations:
Hydrochlorothiazide 25 mg/Spironolactone 25 mg
- Dosage: Initial 1/2 tab/day; Max. 4 tab/day
Hydrochlorothiazide 25 mg/Triamterene 37.5 mg
- Dosage: Initial 1 tab/day; Max. 2 tab/day
Hydrochlorothiazide 50 mg/Amiloride 5 mg
- Dosage: Initial 1 tab/day; Max. 2 tab/day
Ace inhibitors and Diuretics
Benazepril 10 mg/Hydrochlorothiazide 12.5 mg
- Dosage: Initial 1 tab/day; Max. 2 tab/day
Captopril 25 mg/Hydrochlorothiazide 15 mg
- Dosage: Initial 1 tab/day; Max. 2 tabs/day
Lisinopril 10 mg/Hydrochlorothiazide 12.5 mg
- Dosage: Initial 1 tab/day; Max. 2 tabs/day
Enalapril 5 mg/Hydrochlorothiazide 12.5 mg
- Dosage: Initial 1 tab/day; Max. 2 tab/day
Angiotensin receptor blockers and Diuretics
Losartan 50 mg/Hydrochlorothiazide 12.5 mg
- Dosage: Initial 1 tab/day; Max. 2 tab/day
Candesartan 16 mg/Hydrochlorothiazide 12.5 mg
- Dosage: Initial 1 tab/day; Max. 2 tab/day
Irbesartan 150 mg/ Hydrochlorothiazide 12.5 mg
- Dosage: Initial 1 tab/day; Max. 2 tab/day
Valsartan 80 mg/Hydrochlorothiazide 12.5 mg
- Dosage: Initial 1 tab/day; Max. 2 tab/day
Beta-adrenergic blockers and Diuretics
Atenolol 50 mg/Chlorthialidone 25 mg
- Dosage: Initial 1 tab/day; Max. 2 tab/day
Pindolol 10 mg/Hydrochlorothiazide 25 mg
- Dosage: Initial 1 tab/day; Max. 2 tab/day
Metoprolol 50 mg/Hydrochlorothiazide 25 mg
- Dosage: 1 tab once or twice daily; Max. 2 tab
Propranolol 40 mg/Hydrochlorothiazide 25 mg
- Dosage: 2 tab BID; Max. 3 tab
Central alpha/Adrenergic agonist and Diuretics
Methyldopa 250 mg/Hydrochlorothiazide 15 mg
- Dosage: Initial 1 tab PO BID; Max. 4 tab
Calcium channel blockers and Ace inhibitors
Amlodipine 2.5 mg/Benazepril 10 mg
- Dosage: Initial 1 cap daily; Max. 4 cap/day
Felodipine 5 mg/Enalapril 5 mg
- Dosage: Initial 1 tab daily; Max. 3 tab/day
Verapamil extended-release 180 mg/Trandolapril 2 mg
- Dosage: Initial 1 tabs daily; Max. 3 tab/day
Perindopril arginine and Amlodipine
- Dosage: initiated at the recommended starting dose of 3.5 mg/2.5mg once daily; After four weeks of treatment, the dose may be increased to 7 mg/5 mg once daily in adult patients whose blood pressure is not at the appropriate target. If necessary, titration to 14 mg/10 mg once daily may be considered in adult patients insufficiently controlled after four weeks of treatment with 7 mg/5 mg
- Not indicated for the initiation of treatment in elderly patients (> 65 years of age)
Calcium channel blockers and Angiotensin II receptor blocker
Amlodipine (mg)/Telmisartan (mg)
- Dosage: 40/5, 40/10, 80/5 and 80/10 are all available
Direct renin inhibitor and Diuretics
Aliskiren 150/Hydrochlorothiazide 12.5
- Dosage: Initial 1 tab daily; Max. 2 tab/day
[/cq_vc_tab_item][/cq_vc_tabs]
Clinical Trials
- LIFE Cardiovascular morbidity and mortality in the Losartan Intervention For Endpoint reduction in hypertension study (LIFE): a randomized trial against Atenolol
- ACCOMPLISH Avoiding Cardiovascular Events through Combination Therapy in Patients Living with Systolic Hypertension
- HYVET Hypertension in the very elderly
Pipeline Agents
- APOLLO: A Randomized Controlled Trial of Aliskiren in the Prevention of Major Cardiovascular Events in Elderly People
- ALTITUDE: Studying aliskiren on top of ACE-inhibitor or angiotensin-receptor-blocker (ARB) therapy in patients with type 2 diabetes and renal impairment compared with a placebo add-on
Physician Resources
1. Tips for Patient Care
Risk factor management:
Patients with hypertension have a high risk of recurrent MI and stroke
- Emphasize risk factor management (hypertension, DM, obesity etc.)
- Reinforce early smoking cessation
- Adherence to the medications
Medications:
- Advise patient to establish a daily routine for pill-taking
- Simplify the medication regimen to improve compliance
- Consider the use of combination pills
- Consider concurrent risk factors and disease states with the prescribed therapy (e.g. a migraine sufferer with hypertension might benefit from a CCB or beta blocker)
- In elderly patients consider lower starting doses to avoid side effects
Social and stress factors:
- Include family or social support in lifestyle modification
- Be aware that erectile dysfunction can occur with some antihypertensives
2. Scales and Table
-
- BMI calculation:

- Waist circumference (recommended):
- <102 cm (40 in.) for men
- <88 cm (35 in.) for women
Specific Paradigms for Treatment of Hypertension:
References
Core Resources:
- Butalia S, Audibert F, Côté AM, et al. Hypertension Canada’s 2018 Guidelines for the Management of Hypertension in Pregnancy. Can J Cardiol. 2018;34:526-531. doi: 10.1016/j.cjca.2018.02.021. Epub 2018 Mar 1
- Canadian Hypertension Education Program 2013 guidelines; www.hypertension.ca
- Compendium of Pharmaceuticals and Specialties (CPS). Canadian Pharmacist Association. Toronto: Webcom Inc. 2012
- Day RA, Paul P, Williams B, et al (eds). Brunner & Suddarth’s Textbook of Canadian Medical-Surgical Nursing. 2nd ed. Philadelphia: Lippincott Williams and Wilkins; 2010
- Foster C, Mistry NF, Peddi PF, Sharma S, eds. The Washington Manual of Medical Therapeutics. 33rd ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2010
- Gray J, ed. Therapeutic Choices. Canadian Pharmacists Association. 6th ed. Toronto: Webcom Inc. 2011
- Grundy SM, Cleeman JI, Bairey Merz CN, et al, for the Coordinating Committee of the National Cholesterol Education Program. Implications of recent clinical trials for the National Cholesterol Education Program Adult Treatment Panel III guidelines. Circulation. 2004; 110:227-239
- Hurst’s the Heart Manual of Cardiology, 12th Edition
- Katzung BG, Masters SB, Trevor AJ, eds. Basic and Clinical Pharmacology. 11th ed. New York: McGraw-Hill; 2009
- Leiter LA, Fitchett DH, Gilbert RE, Gupta M, et al. Cardiometabolic Risk in Canada: A Detailed Analysis and Position Paper. Canadian Journal of Cardiology 27 (2011) e1-e33
- Longo D, Fauci A, Kasper D, et al (eds). Harrison’s Principles of Internal Medicine. 18thed. New York: McGraw-Hill; 2011
- McPhee SJ, Papadakis MA, eds. Current Medical Diagnosis & Treatment. 49th ed. New York: McGraw-Hill; 2010
- Nerenberg KA, Zarnke KB, Leung AA, at al. Hypertension Canada’s 2018 Guidelines for Diagnosis, Risk Assessment, Prevention, and Treatment of Hypertension in Adults and Children. Can J Cardiol. 2018;34:506-525 DOI:https://doi.org/10.1016/j.cjca.2018.02.022
- Pagana KD, Pagana TJ eds. Mosby’s Diagnostic and Laboratory Test Reference. 9th ed. St. Louis: Elsevier-Mosby; 2009
- Skidmore-Roth L. ed. Mosby’s drug guide for nurses. 9th ed. St. Louis: Elsevier-Mosby; 2011
- Skidmore-Roth L, ed. Mosby’s nursing drug reference. 24th ed. St. Louis: Elsevier-Mosby; 2011
- Stergiou G, Palatini P, Asmar R, et al. Blood Pressure Measurement and Hypertension Diagnosis in the 2017 US Guidelines. Hypertension 2018;71: 963-965. https://doi.org/10.1161/HYPERTENSIONAHA.118.10853
- Whelton PK, Carey RM, Aronow WS, et al.. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension. 2018; 71: e13-e113. https://doi.org/10.1161/HYP.0000000000000065
Online Pharmacological Resources:
- e-Therapeutics
- Lexicomp
- RxList
- Epocrates
Journals/Clinical Trials:
- Al-Balas M, Bozzo P, Einarson A. Use of diuretics during pregnancy Can Fam Physician. 2009; 55(1): 44-45
- Beckett NS et al. Treatment of hypertension in patients 80 years of age or older (HYVET) NEJM 2008; 358:1887-98
- 2012 CHEP Recommendations for the Management of Hypertension
- Canadian Hypertension Education Program, 2013, www.hypertension.ca
- Canadian Hypertension Education Program. 2011 guideline details: assessment of overall cardiovascular risk. Available at: www.hypertension.ca/assessment-of-overall-cardiovascular-risk. Accessed October 17, 2011
- Cushman WC, Evans GW, Byington RP et al. Effects of intensive blood-pressure control in type 2 diabetes mellitus.N Engl J Med 2010; 362:1575-1585
- Dahlof B, Devereux RB, Kjeldsen SE et al. Cardiovascular morbidity and mortality in the Losartan Intervention For Endpoint reduction in hypertension study (LIFE): a randomized trial against Atenolol. Lancet. 2002;359:995-1003
- Genest J, McPherson R, Frohlich J, et al. 2009 Canadian Cardiovascular Society/Canadian guidelines for the diagnosis and treatment of dyslipidemia and prevention of cardiovascular disease in the adult – 2009 recommendations. Can J Cardiol 2009; 25;567-579
- The 7th Report of the Joint National Committee (JNC-7) on Prevention, detection, evaluation and treatment of high blood pressure. JAMA 2003: 289; 2560-71
- Kenneth J, et al. Avoiding Cardiovascular Events through Combination Therapy in Patients Living with Systolic Hypertension (ACCOMPLISH) N Engl J Med 2008; 359:2417-2428
- Okin PM, Wachtell K, Kjeldsen SE, et al. Incidence of atrial fibrillation in relation to changing heart rate over time in hypertensive patients: the LIFE study. Circ Arrhythm Electrophysiol. 2008 ;1:337-43
- Olsen MH, Wachtell K, Beevers G, et al. Effects of losartan compared with atenolol on lipids in patients with hypertension and left ventricular hypertrophy: the Losartan Intervention For Endpoint reduction in hypertension study. J Hypertens. 2009; 27:567-74
- Olsen MH, Wachtell K, Beevers G, et al. Prognostic importance of hemoglobin in hypertensive patients with electrocardiographic left ventricular hypertrophy: the Losartan Intervention For End point reduction in hypertension (LIFE) study. Am Heart J. 2009; 157:177-84
- Sharma AM. Is There a Rationale for Angiotensin Blockade in the Management of Obesity Hypertension? Hypertension. 2004; 44: 12-19
- The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. NIH Publication No. 04-5230; August 2004