Hypothyroidism
ACKNOWLEDGEMENTS:
Thanks to Dr. Ronald M. Goldenberg, MD, FRCPC, FACE, Staff Endocrinologist, North York General Hospital, ON Canada; Endocrinologist & Medical Co-Director, LMC Endocrinology Centres, Toronto, ON Canada, and Dr. William Semchuk, M.Sc., Pharm.D., FCSHP., Manager, Clinical Pharmacy Services, Regina Qu’Appelle Health Region 14, Regina, SK Canada for their expertise with the initial review of this topic.
[pdf-embedder url=”https://www.educateyourhealth.com/wp-content/uploads/2019/03/Hypothyroidism-Brochure.pdf” width=”750″]
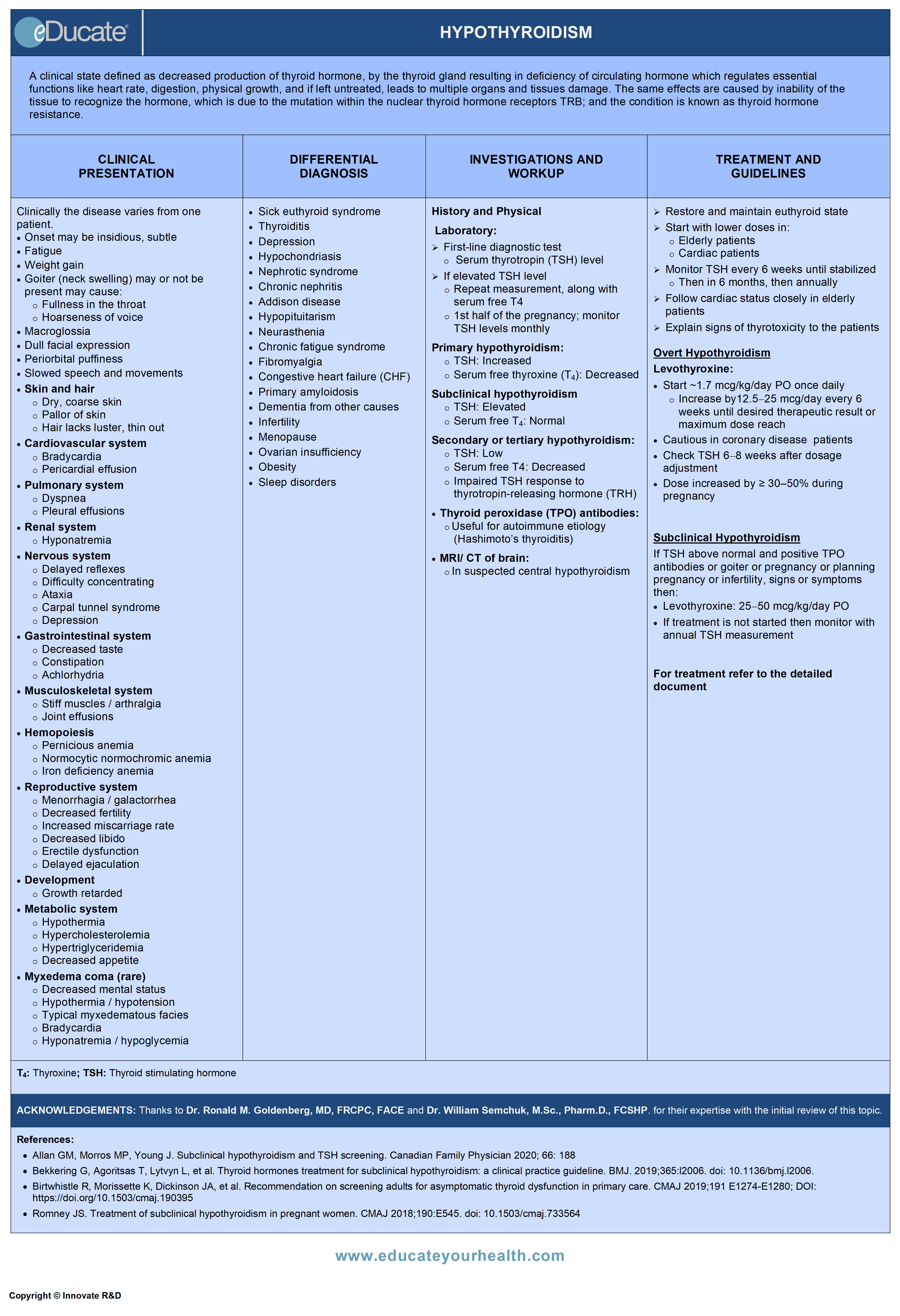
Definition
A clinical state defined as decreased production of thyroid hormone, by the thyroid gland resulting in deficiency of circulating hormone which regulates essential functions; such as heart rate, digestion, physical growth, and if left untreated, leads to multiple organs and tissues damage.
Thyroid hormone resistance: Mutation within thyroid hormone receptors (TRB) leads to poor hormone recognition by tissues and causes a condition similar to low thyroid production state.
Types
Primary hypothyroidism:
- Indicates decreased thyroidal secretion of thyroid hormone by factors affecting the thyroid gland itself
Secondary hypothyroidism:
- Decreased thyroidal secretion of thyroid hormone can also be caused by insufficient stimulation of the thyroid gland by thyroid-stimulating hormone (TSH), due to factors directly interfering with pituitary TSH release.
Tertiary hypothyroidism:
- Indicates decreased thyroidal secretions due to indirect reduction in thyroid releasing hormone (TRH) released from the hypothalamus.
Note: Clinically it is difficult to differentiate between the secondary and tertiary hypothyroidism so they are often collectively referred to as “central hypothyroidism”
Myxedema coma:
A severe state of hypothyroidism which, if left untreated, leads to severe stress and infections.
- Myxedema coma is a potentially lethal but rare condition, occurring with severe hypothyroidism
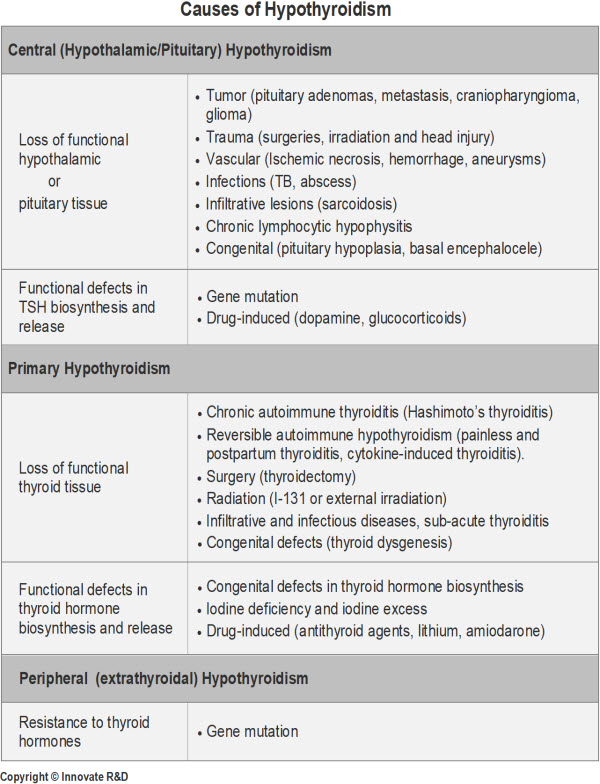
Etiology
Various functional or structural disorders are involved which may cause hypothyroidism, and are categorized as follows:
Primary hypothyroidism:
- Deficient thyroid hormone production by thyroid gland. Usually inherited. Accounts for approximately 90-95% of hypothyroidism
Central hypothyroidism:
- Inadequate stimulation of the normal gland from defect at the level of pituitary or hypothalamus
Peripheral (extrathyroidal) hypothyroidism:
- Symptoms exhibiting hypothyroid state, despite normal structure and function of the thyroid gland and due to peripheral tissue resistance to thyroid hormone
Epidemiology
Incidence
- Predominant age: >40 years
- Predominant gender: Female > Male, 5:1-10:1
Prevalence
- 5-10/1,000 in general population
- Common in elderly
- >65 years of age, increases to
- 6-10% of women
- 2-3% of men
Hashimoto’s thyroiditis:
- Annual incidence
- Women: 400 per 100,000
- Men: 100 per 100,000
- Mean age at diagnosis: 60 years
- Commonest cause of hypothyroidism
Pathophysiology
- Hypothyroidism results from dysfunction in the normal homeostasis in the formation and regulation of the active form of thyroid hormone T3
- Thyroid hormone deficiency may stem from a variety of causes including destruction/atrophy of the thyroid gland (primary hypothyroidism), pituitary insufficiency (secondary hypothyroidism) or from abnormalities of the hypothalamic-pituitary axis (tertiary hypothyroidism)
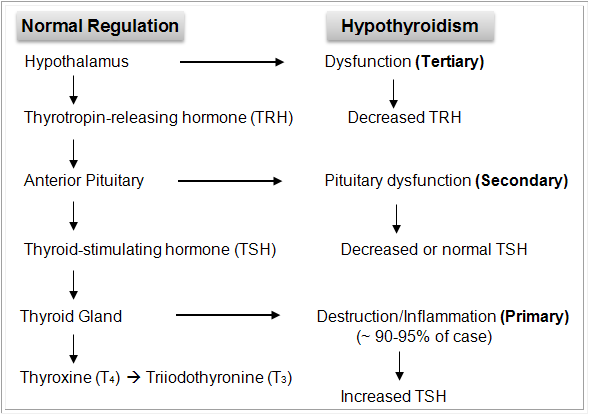
In primary hypothyroidism, in response to a drop in T4 secretion from the thyroid gland, TSH secretion from the pituitary is increased. Thus, an elevated TSH is the primary marker of primary hypothyroidism.
Clinical Presentation
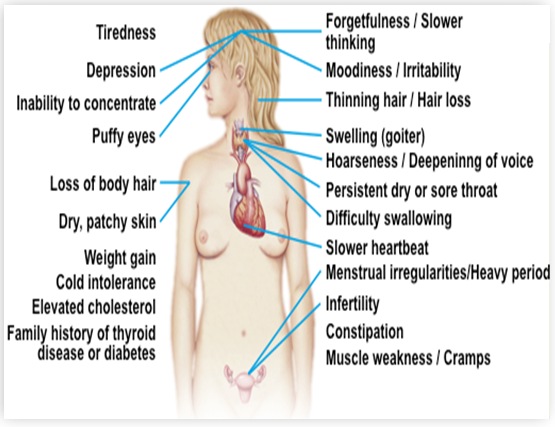
Clinically the disease varies from one patient to the other depending upon cause, duration, and severity of the hypothyroid state. Since thyroid hormones influence most organs, tissues, and cells of the body, there can be a wide spectrum of sign and symptoms in this disorder (see figure).
Note: An endocrinologist would most likely recognize the subtle manifestations and would be more skilled to do physical thyroid gland examination. Consultation is recommended for:
- Patients of age ≤18 years
- Patients who do not respond to treatment
- Pregnant patients
- Cardiac patients
- Structural changes in the thyroid gland
- Presence of other endocrine diseases
Differential Diagnosis
- Sick euthyroid syndrome
- Thyroiditis
- Depression
- Hypochondriasis
- Nephrotic syndrome
- Chronic nephritis
- Addison’s disease
- Hypopituitarism
- Neurasthenia
- Chronic fatigue syndrome
- Fibromyalgia
- Congestive heart failure (CHF)
- Primary amyloidosis
- Dementia from other causes
- Infertility
- Menopause
- Ovarian insufficiency
- Obesity
- Sleep disorders
Investigation and Workup
History and Physical:
History and physical examination will provide definitive information in severe cases, but the disease can often be asymptomatic or have non-specific signs and symptoms. However; biochemical proof of thyroid hormone deficiency is necessary for diagnosis.
Laboratory studies:
- Common tests of thyroid function include TSH, free T4, anti-thyroid peroxidase (anti-TPO) antibodies (see figure)
- Serum thyrotropin hormone (TSH) measurement is the first-line diagnostic test
- An elevated TSH level should be confirmed by a repeated measurement, along with measurement of serum free T4 estimates
- Many patients with primary hypothyroidism have normal circulating levels of T3
- Free T4 assays can be unreliable in the setting of severe illness
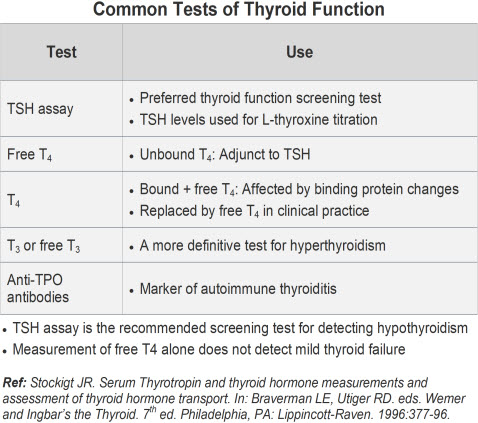
Interpretation of test results:
Although most laboratories report the upper range of normal for TSH is 4.5 mIU/L, evidence suggests that the true upper limit of normal may be as low as 2.5 mu/L.
Ref: Wartofsky, L. The evidence for a narrower thyrotropin reference range is compelling. The Journal of Clinical Endocrinology & Metabolism, 90:5483-5488, 2005.
Overt primary hypothyroidism:
- TSH: Increased
- Serum free thyroxine (T4): Decreased
Subclinical hypothyroidism:
- TSH: Elevated (usually <10 mlU/L)
- Serum free T4: Normal
Secondary or tertiary hypothyroidism:
- TSH: Low or normal
- Serum free T4: Decreased
- Impaired TSH response to TRH
Antithyroid antibodies:
Anti-Thyroid peroxidase (TPO) antibodies
- Useful to establish an autoimmune etiology of hypothyroidism in selected cases
- Useful in predicting progression of subclinical to overt hypothyroidism
Imaging Studies
Ultrasound (thyroid):
- Detect nodules and infiltrative disease
- Useful in follow-up for the size of thyroid and nodules
MRI of the pituitary gland/hypothalamus:
- When central hypothyroidism is suspected
Treatment
Goals: Restore and maintain euthyroid state as reflected by TSH levels.
Agent of choice:
- Levothyroxine once daily, on an empty stomach
- Recommend: High quality (same brand) of levothyroxine to be prescribed throughout the therapy, the reason being bioequivalence and brand interchangeability has not been proven among different brands
Treatment: Is individualized considering age, weight and cardiac status (see figure below)
Monitor treatment: Every 6 to 8 weeks until TSH is normalized, then at 6 months initially followed by annual assessments.
Drugs that interfere with thyroid hormone absorption:
- Iron
- Calcium carbonate
- Cholestyramine
- Lithium
- Aluminum hydroxide gel
- Sucralfate
- Dietary soy
Medical conditions that may interfere with thyroid hormone absorption:
- Gastrointestinal malabsorptive disorders
- Previous small-bowel bypass surgery
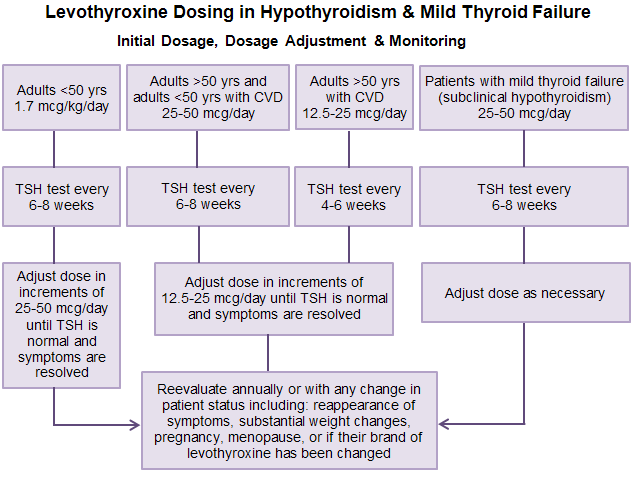
b) Management of subclinical hypothyroidism:
Individuals having a mild increase in TSH (usually <10 mUI/L), with normal free T4 and T3, and who may or may not be symptomatic; ~3-20% of these cases, may progress to (overt hypothyroidism)
Treatment is indicated in patients with:
– TSH >10 mIU/ml
– TSH above normal (4.5 to 10 mUl/L) with a goiter or anti-TPO antibodies, pregnancy, infertility, signs or symptoms or evidence of atherosclerotic cardiovascular disease, heart failure, or risk factors for these diseases
Levothyroxine:
- Starting dosage: 25-50 mcg/d (see figure)
- Monitor TSH in 6-8 weeks and the dose should be adjusted accordingly
- Target TSH value is between 0.3-3.0 mIU/ml
- Once the disease is stabilized annually asses the patient
c) Management of Hypothyroidism during Pregnancy:
Hypothyroidism in pregnancy is associated with:
- Preeclampsia
- Anemia
- Postpartum hemorrhage
- Cardiac ventricular dysfunction
- Spontaneous abortion
- Low birth weight
- Impaired cognitive development
- Fetal mortality/ stillbirths
➣ Increased dosage requirements should be anticipated during pregnancy
- Especially in the first and second trimesters
➣ Women with a history of treated hypothyroidism who are contemplating pregnancy should be rendered euthyroid with a goal TSH no higher than 2.5mUI/L before conception
➣ Patients with hypothyroidism should increase the levothyroxine dose by 30% to 50% by four to six weeks gestation
➣ For previously diagnosed women, serum TSH levels should be measured:
- Every 4 weeks during the first half of pregnancy
- At least once between 26 and 32 weeks gestation
- At 6 weeks postpartum
➣ Levothyroxine dose should be adjusted:
- To maintain a serum TSH less than 2.5 mIU/L, in the first trimester and <3.0 mUI/L in the second and third trimesters
- The dose of levothyroxine may be returned to preconception levels immediately postpartum
References:
- DeGroot L, Abalovich M, Alexander E, et al. Management of thyroid dysfunction during pregnancy or postpartum: An Endocrine Society clinical practice guideline. Journal of Clinical Endocrinology & Metabolism, 2012; 97:2543-2565
- Romney JS. Treatment of subclinical hypothyroidism in pregnant women. CMAJ 2018,30;190:E545. doi: 10.1503/cmaj.733564
- Stagnaro-Green A, Abalovich M, Alexander E, et al. Guidelines of the American Thyroid Association for the diagnosis and management of thyroid disease during pregnancy and postpartum. Thyroid. 2011;21:1-45
d) Hypothyroidism and concurrent diseases:
Diabetes mellitus:
- Approximately 10% of type1 diabetes mellitus patients will develop chronic thyroiditis in their lifetime
- Patients with diabetes should always be examined for goiter and regular TSH level monitoring should be done
- Approximately 25% of women with type1 diabetes mellitus will develop postpartum thyroiditis
Infertility:
Typically patients seek medical attention for infertility or previous miscarriages, when investigated by a careful history, examination and labs will demonstrate clinical or subclinical hypothyroidism.
- Patients with increased TSH levothyroxine replacement therapy will normalize the fertility issues
Depression:
In patients with depression, clinical and subclinical hypothyroidism should always be considered.
- Appropriate levothyroxine doses should be initiated in patients with elevated TSH levels
e) Management of myxedema coma: (Endocrine emergency)
- Myxedema coma is an endocrine emergency and should be treated aggressively
- Any precipitating factors should be treated
- Administer mechanical ventilation if necessary
- Parenteral hydrocortisone (50 mg every 6 hours)
- Until coexisting adrenal insufficiency excluded
- Intravenous Hypertonic saline and glucose
- For severe Hyponatremia or hypoglycemia
- Passive correction of hypothermia
- Active correction can cause vasodilatation and hypotension
Preferred treatment:
- Levothyroxine
- 500 mcg IV, as a one-time loading dose
- Subsequent daily dose: 50-100 mcg
Alternative treatment 1:
- Tri-iodothyronine, T3
- IV or via nasogastric tube, 10-25 mcg every 8-12 hours
- Excess T3 may provoke arrhythmias
Alternative treatment 2:
- Combined Levothyroxine (T4) and Tri-iodothyronine (T3)
- Initial IV bolus levothyroxine (200 mcg) Tri-iodothyronine (25 mcg)
- Subsequent daily doses of levothyroxine (50-100 mcg) and T3 (10 mcg every 8 h) until the patient responds
[/cq_vc_tab_item][cq_vc_tab_item tabtitle=”Medication Dose”]Thyroid agents
- ➣ Levothyroxine
Mechanism
- Exact mechanism of action is unknown
- It is generally believed that they exert its many actions through control of DNA transcription and, ultimately, protein synthesis
- Levothyroxine (T4) is a synthetic form of thyroxine, an endogenous hormone secreted by the thyroid gland. T4 is metabolically deiodinated to active metabolite, L-triiodothyronine (T3) in peripheral tissues
Dose:
Levothyroxine:
- Usual initial dose ~1.7 mcg/kg/day PO once daily; usual doses are ≤200 mcg/day; may titrate dose by 12.5-25 mcg (every 6-8 weeks); Max. 300 mcg/day
Age >50 years or <50 years with the cardiac disease
- Usual initial dose is 25-50 mcg/day; may titrate dose at 6-8 weeks intervals, as needed
Age >50 years with cardiac disease
- Usual initial dose is 12.5-25 mcg/day; may titrate dose at 4-6 weeks interval, as needed
Subclinical hypothyroidism
- Start with 25-50 mcg/day; may titrate dose at 6-8 week intervals as needed
[/cq_vc_tab_item][/cq_vc_tabs]
Clinical Trials
- The starting dose of levothyroxine in primary hypothyroidism treatment: a prospective: randomized, double-blind trial
- The beneficial effect of L-thyroxine on cardiovascular risk factors, endothelial function, and quality of life in subclinical hypothyroidism: randomized, crossover trial
- Subclinical hypothyroidism is associated with increased risk for all-cause and cardiovascular mortality in adults
Pipeline Agents
Pending new data.
Physician Resources
1. Tips for patient care
Risk factor management:
- Advise patient to report signs of infection or potential heart problems (palpitations, dyspnea)
- Hypothyroidism could increase the risk of infertility and miscarriage
- If suspecting the presence of adrenal insufficiency, it should be confirmed or ruled out and should be treated prior to treatment of hypothyroidism
- Generally, routine surgery in a hypothyroid patient should be deferred until euthyroidism is restored
- Diabetic patients may need a readjustment of hypoglycemic agents with the institution of thyroxine
- High-bulk diet may help avoid constipation
- Educate patient about myxedema coma
Monitoring:
- Monitor TSH levels every 6 to 8 weeks until normalized, then at 6 months, followed by annual assessments
- An elevated TSH level should be confirmed by a repeated measurement, along with measurement of serum free T4
- If treatment in subclinical hypothyroidism is not initiated, then monitor with annual TSH and free T4 measurement
- Follow cardiac status closely in elderly patients
Medications:
- Advise patient to establish the prescribed routine for pill-taking
- Educate about the importance of drug therapy compliance
- Appreciate lower starting doses of drugs in elderly and debilitated patients
- Consider concurrent risk factors and disease states with the prescribed therapy
- Levothyroxine is usually the first choice of treatment
- Thyroid hormone has a narrow toxic-to-therapeutic ratio
- Must be titrated on the basis of laboratory tests and clinical responses
- Avoid over-replacement with thyroid hormone
Social and Stress factors:
- Ensure patient and family are well informed about the disease and its treatment
- Individuals with hypothyroid should be regularly screened for subclinical psychological distress and psychiatric disorders
Alerts:
- Iron supplements frequently decrease levothyroxine absorption; caution required especially when iron supplements are prescribed due to increased demand for iron during pregnancy
- Thyroid hormone replacement can precipitate adrenal crises in patients with untreated adrenal insufficiency
- Relapses will occur if treatment is interrupted
Activities (physical, mental, others):
- Stress on the importance of staying active and having a regular exercise routine
- Advise patients to keep themselves mentally active
Myxedema coma:
- Myxedema coma is a medical emergency
- Untreated hypothyroidism may progress to myxedema coma
- Identify and treat the precipitating factors of myxedema coma, such as hypoglycemia, infection, medications, cold exposure
- A random cortisol level should be drawn prior to therapy
- Administer hydrocortisone until coexisting adrenal insufficiency is ruled out
- Deterioration of the patient’s mental status is one of the key manifestations of myxedema coma
Hypothyroidism and Pregnancy:
- Hypothyroidism in pregnancy is safely and easily treated with synthetic thyroid hormone
- Uncontrolled hypothyroidism during pregnancy can lead to, e.g.
- Congestive heart failure, preeclampsia, miscarriage, low birth weight
- Cognitive and developmental disabilities in the newborn
- Levothyroxine requirements will likely increase during pregnancy. Monitor TSH level every 4-6 weeks during the first half of pregnancy and at least once between 26 and 32 weeks gestation
- Women with hypothyroidism should achieve good control prior to conception (TSH not more than 2.5mlU/L)
- After delivery, most patients need to decrease the thyroxine dosage they received during pregnancy
- There is an increased risk of developing permanent primary hypothyroidism in women with a history of postpartum thyroiditis
2. Scales and Table
References
Core Resources:
- Allan GM, Morros MP, Young J. Subclinical hypothyroidism and TSH screening. Canadian Family Physician 2020; 66:188
- American Association of clinical endocrinologist Medical guidelines for clinical practice for the evaluation and treatment of hyperthyroidism and hypothyroidism, 2006 amended version. Endocrine practice Vol 8 No.6
- Bekkering G, Agoritsas T, Lytvyn L, et al. Thyroid hormones treatment for subclinical hypothyroidism: a clinical practice guideline. BMJ. 2019;14;365:l2006. doi: 10.1136/bmj.l2006
- Birtwhistle R, Morissette K, Dickinson JA, et al. Recommendation on screening adults for asymptomatic thyroid dysfunction in primary care. CMAJ 2019; 191:E1274-E1280; doi: https://doi.org/10.1503/cmaj.190395
- Braverman LE, Utiger RD, eds. Werner and Ingbar’s The Thyroid. 9th ed. Philadelphia: Lippincott Williams & Wilkins; 2005
- Compendium of Pharmaceuticals and Specialties (CPS). Canadian Pharmacist Association. Toronto: Webcom Inc. 2012
- Day RA, Paul P, Williams B, et al (eds). Brunner & Suddarth’s Textbook of Canadian Medical-Surgical Nursing. 2nd ed. Philadelphia: Lippincott Williams and Wilkins; 2010
- Foster C, Mistry NF, Peddi PF, Sharma S, eds. The Washington Manual of Medical Therapeutics. 33rd ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2010
- Gray J, ed. Therapeutic Choices. Canadian Pharmacists Association. 6th ed. Toronto: Webcom Inc. 2011
- Katzung BG, Masters SB, Trevor AJ, eds. Basic and Clinical Pharmacology. 1st ed. New York: McGraw-Hill; 2009
- Longo D, Fauci A, Kasper D, et al (eds). Harrison’s Principles of Internal Medicine. 18th ed. New York: McGraw-Hill; 2011
- Management of thyroid dysfunction during pregnancy and postpartum. An endocrine society clinical practice guidelines. 2007 J Clin Endocrinol Metab:92; S1-S47
- McPhee SJ, Papadakis MA, eds. Current Medical Diagnosis & Treatment. 49th ed. New York: McGraw-Hill; 2010
- Pagana KD, Pagana TJ eds. Mosby’s Diagnostic and Laboratory Test Reference. 9th ed. St. Louis: Elsevier-Mosby; 2009
- Romney JS. Treatment of subclinical hypothyroidism in pregnant women. CMAJ 2018;190:E545. doi: 10.1503/cmaj.733564
- Skidmore-Roth L. ed. Mosby’s drug guide for nurses. 9th ed. St. Louis: Elsevier-Mosby; 2011
- Skidmore-Roth L, ed. Mosby’s nursing drug reference. 24th ed. St. Louis: Elsevier-Mosby; 2011
Online Pharmacological Resources:
- e-Therapeutics
- Lexicomp
- RxList
- Epocrates
Journals/Clinical Trials:
- Abalovich M, et al: Management of thyroid dysfunction during pregnancy and postpartum: an Endocrine Society Clinical Practice Guideline. J Clin Endocrinol Metab 2007;92:S1-S47
- American Association of Clinical Endocrinologists medical guidelines for clinical practice for the evaluation and treatment of hyperthyroidism and hypothyroidism. Endocr Pract. 2002;8:457-469
- American College of Physicians. Clinical guideline, part 1. Screening for thyroid disease. Ann Intern Med. 1998;129:141-3
- Alexander EK, Marqusee E, Lawrence J, et al. Timing and magnitude of increases in levothyroxine requirements during pregnancy in women with hypothyroidism. N Engl J Med. 2004;351:241-9
- Assessment of iodine deficiency disorders and monitoring their elimination. A guide for programme managers. (3rd edition). World Health Organization 2007
- Aoki Y, Belin RM, Clickner R, et al. Serum TSH and total T4 in the United States population and their association with participant characteristics: National Health and Nutrition Examination Survey (NHANES 1999-2002). Thyroid. 2007;17:1211-23
- Bunevicius R, Kazanavicius G, Zalinkevicius R, et al. Effects of thyroxine as compared with thyroxine plus triiodothyronine in patients with hypothyroidism. N Engl J Med. 1999;340:424-429
- Cappola AR, Fried LP, Arnold AM, et al. Thyroid status, cardiovascular risk, and mortality in older adults. JAMA 2006; 295:1033-1041
- Cinemre H, Bilir C, Gokosmanoglu F, et al. Hematologic effects of levothyroxine in iron-deficient subclinical hypothyroid patients: a randomized, double-blind, controlled study. J Clin Endocrinol Metab. Jan 2009;94:151-6
- Clyde PW, Harari AE, Getka EJ, Shakir KM. Combined levothyroxine plus liothyronine compared with levothyroxine alone in primary hypothyroidism: a randomized controlled trial. JAMA. 2003; 290:2952-8
- Cooper DS. Subclinical hypothyroidism. N Engl J Med 2001;345:260-265
- Cooper DS, Doherty GM, Haugen BR, Kloos RT, Lee SL, Mandel SJ, et al. Management guidelines for patients with thyroid nodules and differentiated thyroid cancer. Thyroid 2006;16:109-142
- Delange F, de Benoist B, Pretell E, et al: Iodine deficiency in the world: Where do we stand at the turn of the century? Thyroid 2001;11:437-447
- Eskes SA, Endert E, Fliers E, et al. Prevalence of Growth Hormone Deficiency in Hashimoto’s Thyroiditis. J Clin Endocrinol Metab. 2010;95:2266-70
- Escobar-Morreale HF, et al: REVIEW: Treatment of hypothyroidism with combinations of levothyroxine plus liothyronine. J Clin Endocrinol Metab 2005;90:4946-4954
- Garber JR, Hennessy JV, et al: Clinical Update. Managing the challenges of hypothyroidism. J Fam Pract 2006;55:S1-8
- Glinoer D. Management of hypo- and hyperthyroidism during pregnancy. Growth Horm IGF Res. 2003;13 Suppl A:S45-54
- Grozinsky-Glasberg S, Fraser A, Nahshoni E, et al. Thyroxine-triiodothyronine combination therapy versus thyroxine monotherapy for clinical hypothyroidism: meta-analysis of randomized controlled trials. J Clin Endocrinol Metab. 2006;9:2592-9
- Gyamfi C, Wapner RJ, D’Alton ME. Thyroid dysfunction in pregnancy: the basic science and clinical evidence surrounding the controversy in management. Obstet Gynecol. Mar 2009;113:702-7
- Haddow JE, Palomaki GE, Allan WC, Williams JR, Knight GJ, Gagnon J, et al. Maternal thyroid deficiency during pregnancy and subsequent neuropsychological development of the child. N Engl J Med. 1999;341:549-55
- Hollowell JG, Staehling NW, Flanders WD, et al. Serum TSH, T(4), and thyroid antibodies in the United States population (1988 to 1994): National Health and Nutrition Examination Survey (NHANES III). J Clin Endocrinol Metab.2002;87:489-99
- Helfand M. Screening for subclinical thyroid dysfunction in non-pregnant adults: a summary of the evidence for the U.S. Preventive Services Task Force. Ann Intern Med. 2004;140:128-141
- Helfand M, Redfern CC. Clinical guideline, part 2. Screening for thyroid disease: an update. American College of Physicians. Ann Intern Med.1998;129:144-158
- Ito M, Arishima T, Kudo T, Nishihara E, et al. Effect of levo-thyroxine replacement on non-high-density lipoprotein cholesterol in hypothyroid patients. J Clin Endocrinol Metab. 2007;92:608-611
- Kajantie E, Phillips DI, Osmond C, et al. Spontaneous hypothyroidism in adult women is predicted by small body size at birth and during childhood. J Clin Endocrinol Metab. 2006;91:4953-4956
- Kreisman SH, Hennessey JV. Consistent reversible elevations of serum creatinine levels in severe hypothyroidism. Arch Intern Med. 1999;159:79-82
- Ladenson PW. Recognition and management of cardiovascular disease related to thyroid dysfunction. Am J Med. 1990;88:638-641
- Ladenson PW, Singer PA, Ain KB, Bagchi N, Bigos ST, Levy EG, et al. American Thyroid Association Guidelines For Detection Of Thyroid Dysfunction. Arch Internal Med. 2000;160:1573-1575
- LeBeau SO, Mandel SJ. Thyroid disorders during pregnancy. Endocrinol Metab Clin North Am. 2006;35:117-136, vii
- Liu Y. Clinical significance of thyroid uptake on F18-fluorodeoxyglucose positron emission tomography. Ann Nucl Med. 2009;23:17-23
- Morris MS. The association between serum thyroid-stimulating hormone in its reference range and bone status in postmenopausal American women. Bone. 2007;40:1128-1134
- Nebesio TD, McKenna MP, Nabhan ZM, et al. Newborn Screening Results in Children with Central Hypothyroidism. J Pediatr. 2010;156:990-3
- Negro R, Formoso G, Mangieri T, et al. Levothyroxine treatment in euthyroid pregnant women with autoimmune thyroid disease: effects on obstetrical complications. J Clin Endocrinol Metab. 2006;91:2587-2591
- Peleg RK, Efrati S, Benbassat C, et al. The effect of levothyroxine on arterial stiffness and lipid profile in patients with subclinical hypothyroidism. Thyroid. 2008;18:825-30
- Prummel MF, Wiersinga WM. Thyroid autoimmunity and miscarriage. Eur J Endocrinol. 2004;150:751-5
- Razvi S, Ingoe L, Keeka G, et al. The beneficial effect of L-thyroxine on cardiovascular risk factors, endothelial function, and quality of life in subclinical hypothyroidism: randomized, crossover trial. J Clin Endocrinol Metab. 2007;92:1715-23
- Roos A, Linn-Rasker SP, et al. The starting dose of levothyroxine in primary hypothyroidism treatment: A prospective, randomized, double-blind trial. Arch Int Med 2005; 165:1714-1720
- Rosario PW, Bessa B, Valadao MM, et al. Natural history of mild subclinical hypothyroidism: prognostic value of ultrasound. Thyroid. Jan 2009;19:9-12
- Sawin CT, Castelli WP, Hershman JM, McNamara P, Bacharach P. The aging thyroid. Thyroid deficiency in the Framingham Study. Arch Intern Med. 1985;145:1386-8
- Stuckey B, Kent G, Ward L, et al. Postpartum thyroid dysfunction and the long-term risk of hypothyroidism: results from a 12 year follow-up study of women with and without postpartum thyroid dysfunction. Clin Endocrinol (Oxf). 2010;73:389-95
- Supit EJ, Peiris AN. Interpretation of laboratory thyroid function tests for the primary care physician. South Med J 2002;95:481-485
- Surks MI, Ortiz E, Daniels GH, et al. Subclinical thyroid disease: scientific review and guidelines for diagnosis and management. JAMA. Jan 14 2004;291(2):228-38
- Thyroid function test: Diagnosis and monitoring of thyroid function disorders in adults.British Columbia guidelines. Effective date; Jan. 2010
- Tseng FY, Lin WY, et al. Subclinical Hypothyroidism Is Associated With Increased Risk for All-Cause and Cardiovascular Mortality in Adults. J Am Coll Cardiol 2012;60:730-7
- Villar H, Saconato H, Valente O, Atallah AN, et al: Thyroid hormone replacement for subclinical hypothyroidism. Cochrane Database Syst Rev. 2007;18:CD003419
- Wartofsky L. Myxedema coma. Endocrinol Metab Clin North Am. 2006;35:687-698,vii-viii
- Yamada M, Mori M. Mechanisms related to the pathophysiology and management of central hypothyroidism. Nat Clin Pract Endocrinol Metab. 2008;4:683-94