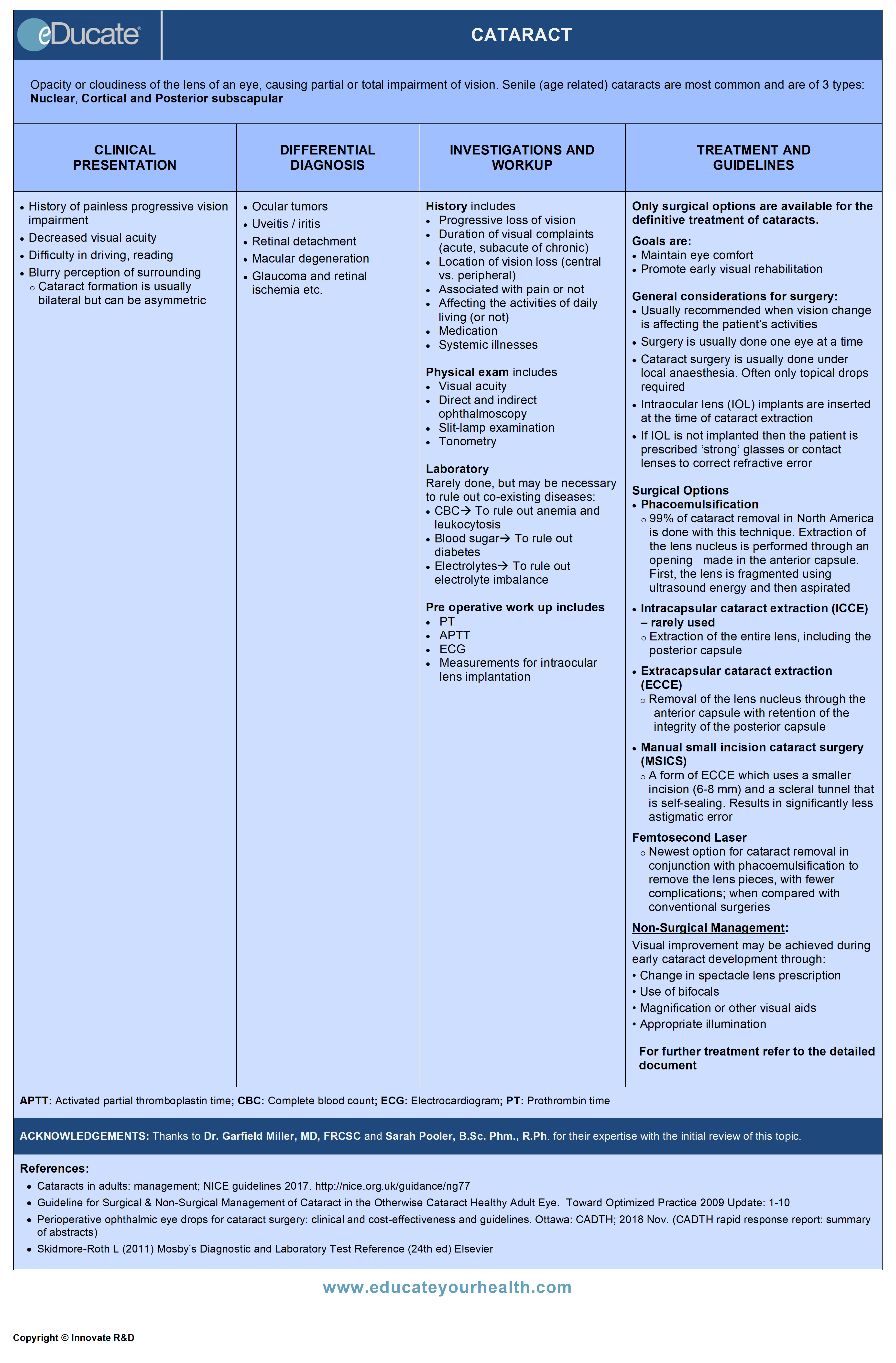
Cataract
ACKNOWLEDGEMENTS:
Thanks to Dr. Garfield Miller, MD, FRCSC, Assistant Professor of Ophthalmology, University of Ottawa, The Ottawa Eye Institute, The Ottawa Hospital, Ottawa, ON Canada, and Sarah Pooler, B.Sc. Phm., R.Ph., Drug Information Pharmacist, Drug Information and Research Centre, Ontario Pharmacists Association, Toronto, ON Canada for their expertise with the initial review of this topic.
Definition
Opacity or cloudiness of the lens of an eye, causing partial or total impairment of vision.
There are 3 most common types of senile (age-related) cataracts; defined by their location within the lens:
- Nuclear: Progression of a yellow to dark brown hue of the lens with increase in density; cause of some nearsightedness as cataract progresses
- Cortical: Located in anterior, posterior or equatorial cortex; cause glare associated with bright lights
- Posterior subscapular: Lies in front of the posterior capsule. Effect on vision can be significant, and often worse with bright lights
- Mixed cataract: More than one type can occur in the same eye
Etiology
Age-Related – most common cause
Systemic diseases
- Diabetes mellitus
- Hypertriglyceridemia
- Renal disorders
- Other metabolic disorders (hypocalcemia, Wilson disease, myotonic dystrophy etc.)
- Atopic dermatitis
- Down syndrome and other chromosomal abnormalities
Ocular disease
- Ocular tumours
- Pathologic myopia
- Uveitis/iritis
- Retinal detachment
- Ocular surgery
- Acute angle closure glaucoma
Environmental factors
- Ultraviolet light
- Radiation
- Smoking
- Trauma
Medications
- Chronic oral corticosteroid use and possibly prolonged administration of high doses of inhaled corticosteroids
- Amiodarone
- Allopurinol
- Phenothiazines
Epidemiology
- From an estimated >30 million blind people worldwide, ~50% is due to cataract
- Senile cataracts represent ~90% of this condition
In Canada
- More than 2.5 million individuals have cataracts, with an anticipated rise to 5 million in 25 years
- By 2031, almost one-quarter of Canadians over the age of 40 will have cataracts
- Prevalence is directly proportional to age
- Percentage according to the age is estimated to be:
- Approx. 2.5% = 40-49 years
- Approx. 25% = 65-69 years
- Approx. 70% = 80 years or more
Pathophysiology
- Lens of the eye is composed of specialized stratified epithelial cells, with high cytoplasmic protein content arranged in a highly complex manner, these proteins provide the transparency to the lens
- The lens is incapable of shedding nonviable cells making it susceptible to degenerative effects of aging
- New cortical layers continuously add in a concentric manner and press and harden the central nucleus
- As the lens ages, its weight increases and accommodation decreases
- The epithelial cells accumulate and lead to loss of transparency
- With aging the rate of transport of water, nutrients, and antioxidants to the lens decrease which potentiates the oxidative processes in cataractogenesis
- Photo-oxidative insult, potentiated by toxic or sensitizing substances, also play a role in the development of opacities
Clinical Presentation
Senile cataracts may be nuclear, cortical or subscapular, affecting different areas of the lens, they may present with different symptoms initially, but the indication for intervention and treatment remains the same.
Broadly may present with:
- History of painless progressive functional impairment in vision
- Cataract formation is usually bilateral but can be asymmetric
- Decreased visual acuity
- Difficulty in driving, reading road signs and reading fine prints
- Excessive glare or decreased vision with bright lights
Late Stages:
- Mature cataract: When the red reflex is lost it is called mature, it degrades vision to the 20/400 level or worse
- Hypermature cataract: It is one in which the cortex of the lens has liquefied (becomes white) and the lens nucleus is mobile within the capsule
Differential Diagnosis
Cataract is essentially the differential for progressive vision loss and might include:
- Ocular tumours
- Uveitis/iritis
- Retinal detachment
- Macular degeneration
- Glaucoma and retinal ischemia etc.
Investigation and Workup
History: Should include the duration of visual complaints, patient’s ability to meet his/ her visual needs and the extent of effect of the deficits; on the daily activities of life.
Inquire about:
- Location of vision loss (central vs. peripheral)
- Progressive loss of vision
- Associated pain (sharp or dull)
Physical exam: The examination should include
- Visual acuity
- Direct and indirect ophthalmoscopy: To rule out retinal disease
- Slit-lamp examination: Detailed visualization of lens opacity
- Tonometry: To rule out increased intraocular pressure
Laboratory:
Rarely done, but may be necessary to rule out co-existing diseases.
- CBC: To rule out anemia and leukocytosis
- Blood sugar: To rule out diabetes
- Electrolytes: To rule out electrolyte imbalance
Preoperative workup:
- PT
- APTT
- ECG
Measurements for intraocular lens implantation include:
- Accurate biometry to calculate the intraocular lens (IOL) power to be used
- Corneal integrity, specifically the endothelial layer, sometimes assessed through pachymetry and specular microscopy to predict postoperative corneal morbidities (e.g. corneal edema, corneal decompensation)
- The power of the IOL on the operated eye must be compatible with the refractive error of the fellow eye to avoid complications (e.g. postoperative anisometropia)
Imaging:
- Ultrasound: Used to rule out posterior segment disease (e.g. ocular tumours or retinal detachment), if the cataract is too dense for direct visualization of back of the eye
Treatment
Goals are:
- Maintain eye comfort
- Promote early visual rehabilitation
Non-Surgical Management:
Visual improvement may be achieved during early cataract development through:
- Change in spectacle lens prescription
- Use of bifocals
- Magnification or other visual aids
- Appropriate illumination
General considerations for surgery:
- Lens removal in cataract patients:
- Usually recommended when vision change is affecting the patient’s activities
- Surgery is usually done one eye at a time
- Cataract surgery is usually done under local anesthesia. Sometimes only topical drops required
- Intraocular lens (IOL) implants are inserted at the time of cataract extraction
- If IOL is not implanted then the patient is prescribed ‘strong’ glasses or contact lenses to correct the refractive error
Contraindications for Surgery:
Cataract surgery is contraindicated when it will not improve visual function due to the presence of coexisting ocular disease
Surgery should not be performed when the patient is unfit for surgery due to underlying systemic disease or coexisting medical conditions
Coexisting conditions in which cataract extraction with IOL implantation are usually contraindicated include:
- Active proliferative diabetic retinopathy (unless cataract removal is necessary to allow visualization of the retina)
- Rubeosis iridis and/or neovascular glaucoma
- Microphthalmos
- Buphthalmos
Surgical Options:
There are currently 4 main surgical options for cataract.
1) Intracapsular cataract extraction (ICCE)
Rarely done anymore. The method involves the extraction of the entire lens, including the lens capsule.
Currently, it is indicated in very few cases, such as; for a dislocated lens with Marfan’s syndrome.
Complications include
- Large incision
- Delayed healing
- Delayed visual rehabilitation
- Significant astigmatism
- Iris incarceration
- Postoperative wound leaks
- Vitreous incarceration
- Corneal edema is a common intraoperative and immediate postoperative complication
2) Extracapsular cataract extraction (ECCE)
This method involves the removal of the lens nucleus through an opening in the anterior capsule with retention of the integrity of the posterior capsule.
ECCE possesses a number of advantages over ICCE:
- A smaller incision ~10-14 mm
- Complications of vitreous adherence to the cornea, iris, and incision are minimized
- Better anatomical placement of the IOL is achieved with an intact posterior capsule
- An intact posterior capsule also
- Reduces the iris and vitreous mobility that occurs with saccadic movements (e.g. endophthalmodonesis)
- Provides a barrier restricting the exchange of some molecules between the aqueous and the vitreous
- Reduces the incidence of CME, retinal detachment, and corneal edema
- Intact capsule prevents bacteria and other microorganisms from gaining access to the posterior vitreous cavity and causing endophthalmitis
- Safer choice for secondary IOL implantation, filtration surgery, corneal transplantation, and wound repairs due to intact posterior capsule
- The main requirement for a successful ECCE and posterior capsule IOL implantation is zonular integrity.
3) Manual small incision cataract surgery (MSICS)
A form of ECCE which uses a smaller incision (6-8 mm) and a scleral tunnel that is self-sealing. Results in significantly less astigmatic error.
4) Phacoemulsification
Extraction of the lens nucleus is performed through an opening made in the anterior capsule. First, the lens is fragmented using ultrasound energy and then aspirated.
Advantages
- Usually requires only topical anesthetic and mild sedation
- Very small incision in the cornea, usually 2-4 mm
- Usually requires one or even no sutures
- Rapid healing
- Rapid visual rehab
- Better control
Lens Replacement:
After the removal of the lens, the patient is referred to as Aphakic (without lens). The lens must be replaced in order to focus light on the retina for patient to see clearly.
There are three lens replacement options:
- Aphakic eyeglasses: Heavy, thick, with limited peripheral vision and magnification of seen objects
- Contact lenses: Provide almost normal vision, but needs to be removed occasionally so eyeglasses are still required
- Intraocular lens implants (IOL): Usual approach during cataract surgery, there are certain conditions, such as uveitis or iris damage, where implantation may be done as a second surgery
Femtosecond Laser:
The newest option where laser therapy is adopted for cataract removal, with fewer complications when compared with the conventional surgeries.
It can be used for wounds, opening of the lens and for the segmentation of cataract; in conjunction with phacoemulsification to remove the lens pieces.
Potential Complications of Cataract Surgery:
INTRAOPERATIVE:
- Posterior capsule rupture
- Vitreous loss
- Dropped lens fragments into the posterior chamber
- Iris or corneal damage
- Wound burn
- Malignant glaucoma
EARLY POSTOPERATIVE:
- Acute bacterial endophthalmitis
- A non-infectious inflammation caused by a toxic agent after uneventful surgery and is a complication of anterior chamber surgery.
- Usually begins less than 24 hrs after surgery
- Presents as corneal edema along with pain and reduction in visual acuity
- Managed by topical steroids, but may be hard to distinguish from endophthalmitis
- Corneal edema
- Wound leak
- High intraocular pressure
LATE POSTOPERATIVE:
- Posterior capsular opacification (PCO)
- Up to 50% of patients who have had cataract surgery will develop a haze behind the artificial lens within the first three years after the surgery, and will require a laser procedure
- Chronic endophthalmitis (rare and often subtle complication)
- Posterior capsular opacification
- Chronic inflammation
- Cystoid macular edema
- Retinal detachment
- Lens dislocation
[/cq_vc_tab_item][cq_vc_tab_item tabtitle=”Medication Dose”]MEDICATIONS:
Local Anesthetic, (ophthalmic)
- Proparacaine
- Tetracaine
Mechanisms:
- Prevents initiation and transmission of impulse at the nerve cell membrane by inhibiting Na ion channels and stabilizing neuronal cell membranes
Dose:
Proparacaine:
Ophthalmic surgery
- 1 gtt of 0.5% solution in the eye every 5-10 mins for 5-7 doses
Tonometry, gonioscopy, suture removal
- 1-2 gtt of 0.5% solution in the eye just prior to the procedure
Tetracaine:
Anesthesia of the eye
- Short-term: 1-2 gtt of 0.5% solution in eye pre-procedure
- Prolonged: 1-2 gtt of 0.5% solution in eye every 5-10 mins for 3-5 doses
Adrenergic, vasopressors, (ophthalmic)
- Phenylephrine
Mechanisms:
Stimulates alpha adrenergic receptors with weak beta-adrenergic activity, producing
- Vasoconstriction of the arterioles of the conjunctiva
- Activates the dilator muscle of the pupil to cause contraction
Dose:
Phenylephrine:
Ocular procedures
- 1-2 gtt of 2.5% or 10% solution and may administer after 10-60 mins as required
Mydriatic, cycloplegic and anticholinergic
- Tropicamide
Mechanisms:
- Prevents the sphincter muscle of the iris and the muscle of the ciliary body from responding to cholinergic stimulation
Dose:
Tropicamide:
- 1-2 gtt of 0.5% solution 15 mins prior to examination; may be repeated every 30 mins or as needed
[/cq_vc_tab_item][/cq_vc_tabs]
Physician Resources
- Ensure patient is well informed about the disease and its treatment
- Until the patient decides to have surgery, advise the following to help decrease symptoms:
- Make sure eyeglasses or contact lenses are the most accurate prescription possible
- Improve the lighting as necessary in the home
- Wearing sunglasses in bright light or a broad-brimmed hat to reduce glare
- May use lamps that provide over-the-shoulder lighting
- Limit night driving
- Following surgery, patients should have help at home due to:
- Restricted activity (e.g. bending over and heavy lifting)
- Blurred vision
- American College of Chest Physicians (ACCP) recommend that
- Patients who are receiving aspirin, may continue to receive aspirin around the time of the cataract procedure
- Caution: Alpha-1-antagonists (commonly used for prostate disease and urological conditions)
- Alpha-1-antagonists have a specific association with intraoperative floppy iris syndrome (IFIS), which can significantly increase the risk of intraoperative complications
- The patient visits the doctor the day after surgery and then usually one week and one month later
- Small fraction of mature and hypermature cataracts can give rise to secondary glaucoma
- Patient should contact the doctor, if there is post-operative severe pain and/or decreased vision
- Infection or serious bleeding may develop in the eye post-surgical, which can lead to a loss of vision
- Highly myopic eyes are at increased risk for retinal detachment after cataract surgery
- Post-surgical:
- Wear glasses or eye shield to protect the eye from injury for minimum 1-2 weeks
- Avoid getting water directly into the eye for one week
- Patients should AVOID:
- Rubbing or bumping the operated eye, especially in the first week
- Bending below the waist for 2-3 days
- Strain or lifting anything heavier than 20 lbs., for the first week, after surgery
- Getting constipated (causes straining)
- Usually, patients without preexisting ocular comorbidity, and uncomplicated cataracts, have a postoperative visual acuity of 20/40 or better
- Posterior capsule opacification develops in ~20% of patients, can be treated in the office with a quick laser procedure-YAG (Yttrium Aluminium Garnet) laser capsulotomy-a painless procedure from which patients can resume normal activities immediately
References
Core Resources:
- American College of Eye Surgeons – Guidelines for cataract practice, 2001
- Bellan L, Ahmed IIK, MacInnis B, et al. Canadian Ophthalmological Society evidence-based clinical practice guidelines for cataract surgery in the adult eye. Can J Ophthalmol 2008;43:S7-57
- Buhrmann R, et al. Foundations for a Canadian Vision Health Strategy: Towards Preventing Avoidable Blindness and Promoting Vision Health prepared for the National Coalition for Vision Health. 2007
- Cataracts in adults: management; NICE guidelines 2017. http://nice.org.uk/guidance/ng77
- Compendium of Pharmaceuticals and Specialties (CPS). Canadian Pharmacist Association. Toronto: Webcom Inc. 2012
- Day RA, Paul P, Williams B, et al (eds). Brunner & Suddarth’s Textbook of Canadian Medical-Surgical Nursing. 2nd ed. Philadelphia: Lippincott Williams and Wilkins; 2010
- Foster C, Mistry NF, Peddi PF, Sharma S, eds. The Washington Manual of Medical Therapeutics. 33rd ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2010
- Gray J, ed. Therapeutic Choices. Canadian Pharmacists Association. 6th ed. Toronto: Webcom Inc. 2011
- Guideline for Surgical & Non-Surgical Management of Cataract in the Otherwise Cataract Healthy Adult Eye. Toward Optimized Practice 2009 Update: 1-10
- Longo D, Fauci A, Kasper D, et al (eds). Harrison’s Principles of Internal Medicine. 18thed. New York: McGraw-Hill; 2011
- McPhee SJ, Papadakis MA, eds. Current Medical Diagnosis & Treatment. 49th ed. New York: McGraw-Hill; 2010
- Optometric Clinical Practice Guideline. Care of the Patient with Cataract (Clinical Practice Guideline 8), Reviewed 2004: 1-43
- Perioperative ophthalmic eye drops for cataract surgery: clinical and cost-effectiveness and guidelines. Ottawa: CADTH; 2018 Nov. (CADTH rapid response report: summary of abstracts)
- Pagana KD, Pagana TJ eds. Mosby’s Diagnostic and Laboratory Test Reference. 9th ed. St. Louis: Elsevier-Mosby; 2009
- Skidmore-Roth L. ed. Mosby’s drug guide for nurses. 9th ed. St. Louis: Elsevier-Mosby; 2011
- Skidmore-Roth L, ed. Mosby’s nursing drug reference. 24th ed. St. Louis: Elsevier-Mosby; 2011
Online Pharmacological Resources:
- e-therapeutics
- Lexicomp
- RxList
- Epocrates Online
Journals/Clinical Trials:
- Gong DH, Liu JF, Zhao X, Zhang L. The effect of nursing intervention on preoperative cataract. Medicine (Baltimore). 2018;97(42):e12749. doi:10.1097/MD.000000000001274
- Javitt JC, Wang F, West SK. Blindness Due to Cataract: Epidemiology and Prevention Ann Rev Public Health 1996; 17: 159-177
- Li N, Li W, Liu R, et al. Interventional nursing promotes visual recovery in senile cataract with glaucoma and reduces the incidence of postoperative complications. Int J Clin Exp Med 2019;12(5):5563-5571