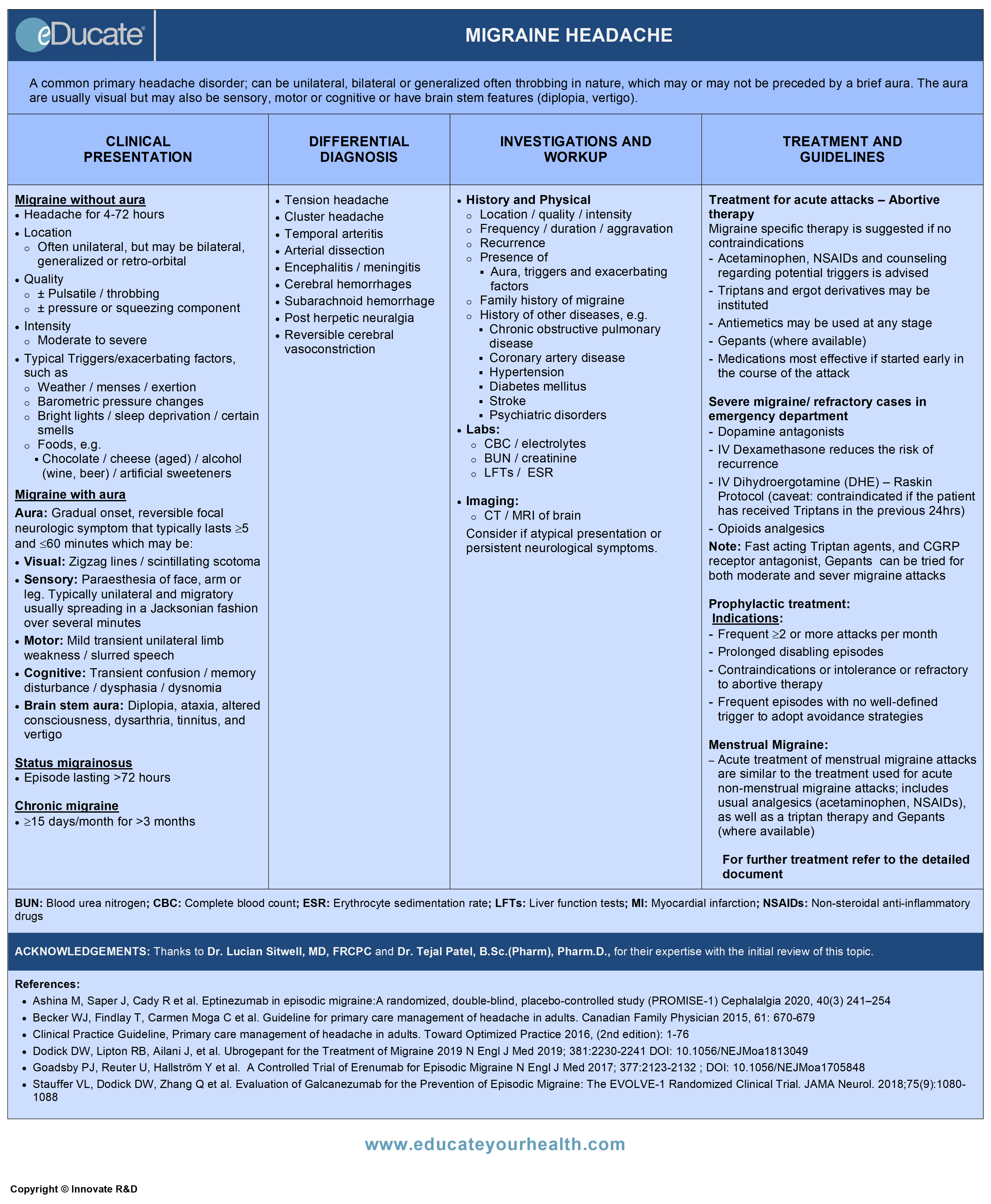
Migraine Headache
ACKNOWLEDGEMENTS:
Thanks to Dr. Lucian Sitwell, MD, FRCPC, Lecturer, University of Ottawa, The Ottawa Hospital-Riverside Campus, ON Canada, and Dr. Tejal Patel, B.Sc.(Pharm), Pharm.D., Clinical Assistant Professor, School of Pharmacy, University of Waterloo, Waterloo, ON Canada for their expertise with the initial review of this topic.
Definition
Unilateral, bilateral or generalized often throbbing headache, which may or may not be preceded by a brief aura. The latter are usually visual but may also be sensory, motor or cognitive or cognitive or have brain stem features (diplopia, vertigo).
Summary of types of migraine:

- Familial hemiplegic migraine (FHM):
- Migraine with aura including motor weakness and at least one first- or second-degree relative has migraine aura including motor weakness. Autosomal dominant associated with mutation has 3 subtypes; FMH1, FMH2, and FMH3
- Sporadic hemiplegic migraine (HM):
- Migraine with aura including motor weakness but no first- or second-degree relative has aura including motor weakness
- Basilar-type migraine (BTM):
- Usually exhibit brain stem symptoms including lightheaded, vertigo, dysarthria, diplopia, ataxia and generalized weakness and decreased level of consciousness. No motor weakness
- Retinal migraine (RM):
- Scotoma or blindness (monocular) lasting less than an hour, with or after headaches
Ref: The International Headaches Classification (ICHD-2) (http://ihs-classification.org).
Etiology
The underlying mechanism(s) remain poorly understood, but appears to involve:
- Neuronal hypersensitivity to physical and environmental stressors, foods and hormonal changes leading to cortical spreading depression (mitigates auras), vascular hypersensitivity and inflammation which causes throbbing focal or generalized pain
- Genetic factors: Autosomal dominant familial hemiplegic migraine provides some evidence of a genetic link to migraine. Other forms of migraine do tend to run in families; 70% of patients have a first-degree relative with a history of migraine
Epidemiology
- Prevalence
- 17-19% women per year in the general population
- 6% men per year in the general population
- Male:Female ratio is 1:3
- May begin at any age, although the incidence of new-onset diminishes with age
- Prevalence peaks at approximately 30-40 years of age for both sexes
Pathophysiology
Aura:
- Cortical spreading depression (CSD) is a self-propagating wave of neuronal and glial depolarization, which spreads across the cerebral cortex and is thought to underlie migraine auras
- CSD may spread sequentially across the cortex e.g. occipital→ parietal → frontal with ensuing sequential symptoms, i.e. visual → sensory → motor
Pain (potential mechanisms):
- Mediated by the trigeminovascular system; extracranial vasodilation results from stimulation of the trigeminal nerve. Neurotransmitters, such as CGRP and substance P are synthesized by ganglion cells and travel to small unmyelinated fibers around the vessels as well as the trigeminal nucleus. Stimulation of the trigeminal ganglion causes vasodilatation and enhanced plasma protein permeability and sterile inflammation. Information is then relayed to the thalamus and cortex for registering of pain. Involvement of other centers may explain the associated autonomic symptoms and affective aspects of this pain
- Cortical spreading depression (CSD) activates trigeminal nerve afferents and alters blood-brain barrier permeability. The activation of trigeminal afferents by CSD, in turn, causes inflammatory changes in the pain-sensitive meninges that generates migraine headache through central and peripheral reflex mechanisms
Clinical Presentation
May present with or without aura
Migraine without aura
- Headache for 4-72 hours
- Location: Often unilateral, but may also be bilateral, generalized or retro-orbital
- Quality: Tends to be, but not always, pulsatile/throbbing ±pressure or squeezing component
- During headache patient may experience any of the following:
- Nausea
- Vomiting
- Photophobia
- Phonophobia
- Intensity: Moderate to severe
- Typical triggers/exacerbating factors:
- Weather/altitude
- Sleep disturbance (excess, deprivation or change)
- Menses
- Exertion
- Certain smells, perfumes, smoke
- Bright lights, loud noises, computer screens
- Foods like chocolate, cheese (aged), alcohol (wine, beer), artificial sweeteners, MSG, processed meats (salami, pepperoni, etc contain nitrates), nuts, citrus, some types of yeast, excess caffeine
Migraine with aura
Often develop gradually over 5-20 mins; may last for less than 60 mins. These are reversible focal neurologic symptom and includes:
- Visual:
- Zigzag lines, scintillating scotoma, visual field defects
- Sensory:
- Paraesthesia of face, arm or leg. Typically unilateral and migratory, usually spreading gradually over several minutes (Jacksonian march)
- Motor:
- Mild transient unilateral limb weakness or slurring of speech
- Cognitive:
- Transient confusion, memory disturbance, dysphasia, dysnomia
- Brain stem aura:
- Diplopia, ataxia, altered consciousness, dysarthria, tinnitus, and vertigo
Note: There are other visual auras, but the ones listed above are the main.
Headache with the features of migraine follows aura usually within 60 minutes; may begin during aura and sometimes>60 minutes post aura. Less commonly headaches lack migrainous features or they may be completely absent.
Other presentations:
- Status migrainosus: Episode lasting >72 hours
- Chronic migraine: Occurs ≥15 days per month for more than 3 months
- Serious complications of migraine: Both seizures and stroke have been associated with migraine
Differential Diagnosis
Investigation and Workup
History and Physical:
Enquire about pain:
- Quality, location, and frequency of headache
- Presence of aura, triggers and exacerbating factors
- Gradual onset; but can occur suddenly
- Recurrence
- Family history of migraine
- Neck examination (assess of neck posture and range of motion, and palpation for muscle tender points)
Labs:
- CBC, electrolytes, BUN, creatinine, LFTs, ESR
CT/MRI-Brain:
- Consider if atypical presentation or persistent neurological symptoms
Treatment
- Severity of headaches
- Associated symptoms and medical conditions
- Frequency, duration, and impact on the quality of life
- Response to medications
- Pregnancy
A) Treatment for acute attacks – Abortive therapy
1) Mild migraine:
- Acetaminophen, NSAIDs, and counseling with regards to potential triggers usually the first course of action, along with the timely institution of triptans, in the early mild phase of migraine
NOTE: Ttriptans may be considered as well; Spectrum study demonstrated in HIS migraine sufferers, triptans were very efficacious in mild head pain and is useful in the early treatment of disabling headaches, rather than later phase of the course.
Ref: Lipton RB, Stewart WF, et al. 2000 Wolff Award. Sumatriptan for the range of headaches in migraine Sufferers. Results of the spectrum study. Headache 2000; 40: 783-91.
2) Moderate to severe migraine course, migraine-specific therapy is recommended if no contraindications
- Medications most effective if started early in the course of the attack
- Triptans and ergot derivatives should be considered for initial therapy or may be used if over the counter analgesics are ineffective
- Calcitonin receptor antagonists (Gepants): Ubrogepant (Ubrelvy), Rimegepant ( Nurtec ODT) may have a role in early abortive therapy in this setting
- Antiemetics may be used at any stage
3) Very severe migraine/ refractory cases in the emergency department
- Dopamine antagonists
- IV Dexamethasone reduces the risk of recurrence within 72 hrs
- IV Dihydroergotamine (DHE) – Raskin protocol (caveat: DHE is contraindicated if the patient has received triptans in the previous 24 hrs)
- Opioids analgesics
Note: Fast-acting Triptan agents, and CGRP receptor antagonist, Gepants can be tried for both moderate and severe migraine attacks, e.g:
- Subcutaneous sumatriptan 6 mg if the patient is vomiting early in the attack. Consider for attacks resistant to oral triptans
- Oral wafer: rizatriptan 10 mg or zolmitriptan 2.5 mg if fluid ingestion worsens nausea
- Nasal spray: zolmitriptan 5 mg or sumatriptan 20 mg If the patient is nauseated
- Gepants: Ubrelvy (ubrogepant) 50 mg or 100 mg orally, Rimegepant (Nurtec ODT) 75 mg orally
- Antiemetics: Metoclopramide 10 mg for nausea
B) Prophylactic treatment:
Indications include
- Frequent ≥2 or more attacks per month
- Prolonged disabling episodes
- Contraindications or intolerance or refractory to abortive therapy
- Frequent episodes with no well-defined trigger to adopt avoidance strategies
Therapy:
In spite of the use of multiple drugs for migraine prophylaxis, many questions regarding the mechanisms of action remain unanswered and require further research.
It might take 4-8 wk for the substantial benefit to occur.
It has been suggested, that there are 2 main targets for migraine prevention:
- Neuronal hyperexcitability
- Nociceptive dysmodulation
The recommended agents for migraine prevention are as follows:
- Antidepressants (amitriptyline, nortriptyline, venlafaxine)
- Anticonvulsants (Divalproex and topiramate)
- Beta-adrenergic blockers (propranolol, timolol, nadolol and metoprolol)
- Calcium channel blockers (verapamil, flunarizine)
- CGRP antagonist (monoclonal antibodies)
- Erenumab (Aimovig): Available in Canada and the USA
- Galcanezumab (Emgality): Available in Canada and the USA
- Fremanezumab (Ajovy): Available in the USA
- Eptinezumab (Vyepti): Available in the USA
Other agents may have some beneficial effect, requiring further research:
- ACE inhibitors
- Angiotensin receptor blockers
- Gabapentin
- Monoamine oxidase inhibitors
- Pizotifen
Factors influencing the choice of migraine prophylactic agents include consideration of comorbidities, potential adverse effects, patient’s expectations or desires, compliance, and cost.
Ref: Ramadan NM, Current Trends in Migraine Prophylaxis. Headache 2007;47:S52-S57)
Menstrual Migraine:
Acute treatment of menstrual migraine attacks is similar to the treatment used for acute non-menstrual migraine attacks; includes usual analgesics (acetaminophen, NSAIDs), as well as a triptan therapy and Gepants (where available).
For severe perimenstrual migraine, refractory to conventional abortive therapy, standard migraine prophylactic agents might be used, particularly if the patient also has non-peri-menstrual migraine episodes as well.
Other treatment strategies include:
- Intermittent short-term prophylaxis with hormonal agents (e.g., estradiol cream 1.5 mg daily for seven days beginning two days before menstruation or estradiol 100 μg patch used in the same way)
- Naproxen
- Short-term prophylaxis with frovatriptan 2.5 mg BID, initiated 2 days before the anticipated menstruation-induced migraine attack and continuing for a total of six days
- Oral contraceptives – continuous use of low-dose combination can be considered, but other treatment options should be tried first
Migraine Treatment in Pregnancy:
- Acetaminophen 1000 mg (up to 4 grams/day) and metoclopramide 10 mg can be used
- Acetaminophen – codeine combination
- Ibuprofen 400 mg can be used for acute migraine attacks during the second trimester of pregnancy. All NSAIDs, including ibuprofen, should be avoided in the first and third trimester of pregnancy
[/cq_vc_tab_item][cq_vc_tab_item tabtitle=”Medication Dose”]MEDICATIONS – ABORTIVE THERAPY
Including, but not limited to the following:
- NSAIDs
- Ibuprofen
- Naproxen
- Aspirin
- Acetaminophen
Mechanism:
NSAIDs:
- Prostaglandin is believed to be a common factor in the production of pain, fever, and inflammation
- NSAIDs inhibit COX-1 and 2 enzymes → result in decreased formation of prostaglandin precursors
Acetaminophen
- Analgesic action: Inhibit the synthesis of prostaglandins in the central nervous system
Dose:
Ibuprofen:
- 200-400 mg PO every 4-6 hrs; Max. 3.2 gm/24 hrs
Naproxen:
- Initial 500-750 mg PO, an addition of 250-500 mg may be given if needed; Max. 1.25 g/24 hrs
Aspirin:
- 325-650 mg PO every 4-6 hrs; Max. 4 g/day
- 300-600 mg rectal suppositories every 4-6 hrs; Max. 4 g/day
Acetaminophen:
- 325-650 mg PO every 4-6 hrs or 1000 mg PO TID or QID; Max. 4 g/day
- Note: Suppositories are used in same doses as of oral formulation.
Warning:
Increased risk of medication overuse/induced headache, if used on more than 8-10 days per month.
Triptan Agents (5-HT1 receptor agonist)
- Sumatriptan
- Zolmitriptan
- Naratriptan
- Almotriptan
- Rizatriptan
- Frovatriptan
- Eletriptan
Mechanism:
- Selective serotonin agonist (5-HT1B/1D receptors)
- Exact mechanism unknown
- Suggested mechanism:
- Inhibit pro-inflammatory neuropeptide release
Dose:
Sumatriptan
- Oral: 25-50 or 100 mg; may repeat after 2 hrs not to exceed 200 mg/day
- Intranasal: 5-20 mg; Max single dose 20 mg; may repeat after 2 hrs, Max. 40 mg/24 hrs
- SC: Single dose of 6 mg; may repeat after 1 hr; Max. 12 mg/24 hrs (2 doses/24 hrs)
Zolmitriptan
- Oral: 2.5 mg; may repeat after 2 hrs; Max. 10 mg/24 hrs
- Intranasal: 2.5-5 mg dose; may repeat after 2 hrs; Max. 10 mg/24 hrs
- May decrease dose of zolmitriptan with concurrent propranolol
Naratriptan
- Oral: 1-2.5 mg; may repeat after 4 hrs; Max. 5 mg/24 hrs
- Mild-moderate renal impairment: Start 1 mg; Max. 2.5 mg/24 hrs
- Hepatic impairment (Child-Pugh Grade A or B): 1 mg; Max. 2.5 mg/24 hrs
Almotriptan
- Oral: 6.25-12.5 mg; may repeat after 2 hrs; Max. 25 mg/24 hrs
- Renal (Clcr ≤30 mL/min) or hepatic impairment: Start 6.25 mg as a single dose; Max. 12.5 mg/24 hrs
- Avoid use if renal impairment and concomitant CYP 3A inhibitor
Rizatriptan
- Oral: 5-10 mg; may repeat dose after 2 hrs; Max. 30 mg/24 hrs
- Patient on Propranolol: 5 mg PO as a single dose; Max. 15 mg/24 hrs
Frovatriptan
- In Canada: 2.5 mg PO; may repeat dose after 4 hrs; Max. 5 mg/24 hrs
- In US: 2.5 mg PO; may repeat after 2 hrs; Max. 7.5 mg/24 hrs
- Menstrual migraine: 2.5 mg, 2 tabs 2 days prior to menses the 1 tab daily for ensuing 5 days
Eletriptan
- Initial 20-40 mg PO; if headache recurs after improving, dose may be repeated after 2 hrs; (Max. single dose is 40 mg, maximum daily dose is 80 mg)
Warning: Increased risk of medication overuse/induced headache, if used on more than 8-10 days per month.
- Ergotamine
- Dihydroergotamine
Mechanism:
- Stimulates alpha-adrenergic and serotonergic (5-HT) receptors
Dose:
Ergotamine:
- 2 mg SL; may repeat dose every 30-60 mins, Max. 6 mg/24 hrs, 10 mg/week
Dihydroergotamine (IM / IV / SC):
- 1 mg at first sign of headache; may repeat dose hourly; Max. 6 mg/week
- Intranasal 1 (0.5 mg) dose into each nostril; may repeat dose after 15 mins, if needed; Max. 6 sprays (3 mg)/24 hour and Max: 8 sprays (4 mg)/week
Intractable migraine (status migrainosus: >72 hrs)
- (IV-Raskin protocol): Initial test dose of 0.5 mg over 2 minutes given after 30 minutes of premedication with IV metoclopramide
- Subsequent dosing is titrated between the range of 0.2-1 mg every 8 hr, for 2-3 days, administered with or without metoclopramide (based on response and tolerance).
- Maximum dose is typically 6 mg/week, but some reports suggest as much as 20 mg/week may be used
Warning: Increased risk of medication overuse/induced headache, if used on more than 8-10 days per month.
- Metoclopramide
- Prochlorperazine
- Chlorpromazine
- Haloperidol
Mechanism:
Metoclopramide
- Blocks dopamine and serotonin receptors in chemoreceptor trigger zone of the CNS
- Enhances the response to acetylcholine of tissue in upper GI tract
Prochlorperazine/chlorpromazine/haloperidol
- Blocks postsynaptic mesolimbic dopaminergic receptors in the brain
- Exhibits a strong alpha-adrenergic and anticholinergic blocking effect
- Depresses the release of hypothalamic and hypophyseal hormones
Dose:
Metoclopramide:
- 10-20 mg PO, IM or IV
Prochlorperazine
- Oral: 5-10 mg 3-4 times/day prn; Max. 40 mg/day
- IM: 5-10 mg every 3-4hrs as needed; Max. 40 mg/day
- IV: 2.5-10 mg; Max. 10 mg/dose or 40 mg/day
- Rectal: 25 mg BID or as needed
Chlorpromazine:
- Oral: 10-25 mg; may repeat dose after 4-6 hrs as needed
- IM: 25 mg (1 mL). If no hypotension occurs, give 25 to 50 mg every 3-4 hrs, until vomiting stops; then switch to oral dosage
- Rectal: One 100 mg suppository every 6-8 hrs. In some patients, half this dose will do
Haloperidol:
- 0.5-2 mg IM or IV
- Tramadol
- Codeine
- Acetaminophen + codeine
- Oxycodone
- Acetaminophen + oxycodone
Mechanism:
- Not fully understood
- Binds to mu opioid receptors in the CNS
- Tramadol: Inhibits serotonin and norepinephrine reuptake in the CNS
Dose:
Tramadol
- Immediate-release: 25-100 mg PO every 4-6 hrs Max. 400 mg/day
- Extended-release 100 mg PO daily; titrate every 5 days, as needed; Max. 300 mg/day
Codeine
- Oral: 30 mg every 4-6 hrs; usual range 15-120 every 4-6 hrs.
- Prior exposure may require higher initial dose
- Controlled release: 50-300 every 12 hrs; should only be considered in chronic or continuous pain, higher doses are used in opioid-tolerant patients
- IM/SC: 30 mg every 4-6 hrs; prior exposure requires higher doses. Usual dose 15-120 mg
- Note: Dose adjustment required in renal/hepatic impairment.
Oxycodone
- Oral: 5-15 mg every 4-6 hrs; range 5-20 mg/dose
- Controlled release: 10 mg every 12hrs; with concurrent CNS depressants decrease dose by 1/3 to 1/2
Warning: Increased risk of medication overuse/induced headache, if used on more than 8-10 days per month.
- Dexamethasone
Mechanism:
Glucocorticoids decrease inflammation through multiple mechanisms, including
- Stabilization of leukocyte lysosomal membranes
- Inhibition of macrophage accumulation
- Reduction of capillary permeability
Dose:
Dexamethasone
- 8-24 mg IV for abortive therapy in ER phase
Calcitonin Gene Related Peptide (CGRP) receptor blockers:
- Ubrogepant (Ubrelvy)
- Rimegepant sulfate (Nurtec ODT)
Indication: Acute treatment of migraine. Approved in USA; not currently available in Canada
Mechanism:
- Block the effect of CGRP through inhibition of the CGRP receptor function
Dose:
Ubrogepant (Ubrelvy)
- For migraine with or without Aura: 50 mg or 100 mg orally
- Side effect: Nausea, somnolence, and dry mouth
Rimegepant sulfate (Nurtec ODT)
- 75 mg orally (rapidly dissolving); beneficial effects may last for 48 hours
- Side effect: Nausea
MEDICATIONS – PROPHYLACTIC THERAPY
Beta-Adrenergic Receptor Blockers
- Cardioselective
- Atenolol
- Metoprolol
- Non-Cardioselective
- Nadolol
- Propranolol
- Timolol
Mechanism:
- Decrease heart rate and cardiac output
- Decrease renin release
- Actual mechanism of migraine prophylaxis unknown
Dose:
Cardioselective:
Atenolol
- Initial 12.5-25 mg PO daily; may gradually increase to 100 mg/day in divided doses
Metoprolol
- Initial 25-50 mg PO BID; may increase 100-200 mg/day
- Max. ~300 mg/day
Non-Cardioselective:
Nadolol:
- Initial 40 mg PO daily; usual 40-120 mg daily; may increase to ~240-320 mg/day
Propranolol:
- Conventional tablets: Start 40-80 mg PO daily in 2-3 divided doses; may increase by 20-40 mg/dose every 3-4 weeks; Max. 160-240 mg/day in divided doses
- Extended-release capsules: Start 80 mg PO daily, usual 160-240 mg/day
Timolol:
- Start 20 mg PO BID; may increase gradually every 7 days; usual dose 20-40 mg PO BID, Max dose is 60 mg/day
- Amitriptyline
- Nortriptyline
- Desipramine
Mechanisms:
- Inhibits the presynaptic reuptake of neurotransmitters → increases synaptic serotonin and/or norepinephrine → potentiates its effect
- Also has significant anticholinergic properties
Dose:
Amitriptyline/Nortriptyline/Desipramine
- Start 10-25 mg PO at bedtime; may increase gradually by 10-20 mg increments weekly as needed; usual maintenance dose 50-75 mg/day at bedtime; Max dose: ~150 mg at bedtime
- Valproate/divalproex
- Topiramate
Mechanisms:
- Exact mechanism is not known, but suggestions include:
- Increased availability of GABA → resulting in seizure activity suppression, decreased manic episodes and decreased frequency of migraine headaches
Dose:
Valproate/divalproex:
- 250 mg/day PO BID; titrate dose based on patient response; Max. 1.5 g/day
Topiramate:
- 25 mg PO daily for 1 week; then increase weekly by 25 mg/day until at 50 mg BID
- Doses >100 mg/day have shown no additional benefit.
- Renal:
- Administer 50% dose and titrate more slowly if ClCr <70 mL/minute/1.73 m2
Selective Calcium Channel Antagonist
- Flunarizine
Mechanism:
- Mediated through blockade of calcium channels
- Also have antihistamine properties (histamine H1 receptors inhibition)
Dose:
Flunarizine
- 5-10 mg PO daily, to minimize the side effects allow 2 medication-free days in a week
Calcitonin gene-related peptide (CGRP) inhibitors (Monoclonal antibodies)
- Erenumab (Aimovig): Available in Canada and USA
- Galcanezumab (Emgality): Available in Canada and USA
- Fremanezumab (Ajovy): Available in USA
- Eptinezumab (Vyepti)
Mechanism:
- CGRP modulates pain. Monoclonal antibodies nullify the effects of the CGRP molecule
Dose:
Erenumab (Aimovig)
- 70 mg subcutaneously once a month; may increase to 140 mg subcutaneously once a month depending on the response to initial dose and tolerance
- Side effects: Constipation; or local injection site irritation
Galcanezumab (Emgality)
- Loading dose: 240 mg subcutaneously then 120 mg subcutaneously monthly
- Side effects: Allergic reaction (hives, swelling shortness of breath); seek urgent medical care. Injection site irritation
Fremanezumab (Ajovy)
- 225 mg subcutaneously once a month OR 675 mg subcutaneously once every 3 months
- Side effects: Allergic reaction (hives, swelling shortness of breath); seek urgent medical care. Injection site irritation
Eptinezumab (Vyepti)
- 100 mg or 300 mg IV infusion every three months
- Side effects: Hypersensitivity reaction; fatigue
Serotonin and Histamine Antagonist
- Pizotifen
Mechanism:
- Is not fully known, in migraine
- It is a competitive serotonin antagonist with antihistamine
- Weak anticholinergic properties
Dose:
Pizotifen
- Start 0.5 mg PO daily at night, increased gradually to maintenance dose of 1.5 mg/day in 3 divided doses; Max. 6 mg/day
Note: May take ~4 weeks to reach its maximum effect.[/cq_vc_tab_item][/cq_vc_tabs]
Clinical Trials
- Spectrum study: Sumatriptan for the range of headaches in migraine Sufferers. Results of the spectrum study
Physician Resources
1. Tips for Patient Care
Ask patients to:
- Diarize headaches and potential triggers (useful in follow-up assessment)
- Identify and avoid triggers
- Lifestyle modifications if required (improve sleep, avoid hunger, wine etc.)
- Be aware of early signs of migraine and promptly initiate abortive therapy
Medications:
- Evaluate cost, affordability and insurance coverage for patients
- Discuss potential adverse events/side effects of medications
- Consider daily prophylaxis for:
- Frequent migraines
- Those with prolonged debilitating episodes lasting days
- Consider concurrent risk factors and disease states when prescribing prophylactic agents e.g.
- A beta-blocker or CCB might be a good choice for a patient with both HTN and migraine
- Topiramate or Valproate might be considered in those with seizure or mood disorders
- Topiramate might also be beneficial in those seeking weight losses
- TCAs might be used to assist sleep and control migraines in patients with sleeping problems
Social and Stress factors:
- Patient & family members should be well informed about disease and its treatment
- Advise to make changes in your work environment that reduces susceptibility to migraine triggers (e.g. use curtains to avoid glare from windows, sit further away from solvents, wear earplugs in noisy environments etc.)
- Advise rest in a quiet, dark room during periods of headache exacerbation
- If headache begins to subside, advise patients to minimize exposure to offending stimuli that might reactivate a migraine
- Advise patients to monitor frequency of attacks, pain location and quality, and medication usage
- Rest and relaxation with regular exercises; may help to reduce tension and prevent migraines
- Avoid frequent daily use of analgesics which might lead to chronic daily headache
Physical activity:
- Patients should be aware that vigorous activity can potentiate migraines (“exercise-induced migraines”), but at the same time, regular moderate exercise can decrease migraine frequency. If this occurs, advise to pre-treat with analgesics before physical activity. This may abort headache occurrence or blunt a headache caused by activity
2. Scales and Tables:
References
Core Resources:
- Brust JCM (2007) Current Diagnosis and Treatment (Neurology) (2nd ed.) New York: McGraw Hill
- Compendium of Pharmaceuticals and Specialties (CPS). Canadian Pharmacist Association. Toronto: Webcom Inc. 2012
- Day RA, Paul P, Williams B, et al (eds). Brunner & Suddarth’s Textbook of Canadian Medical-Surgical Nursing. 2nd ed. Philadelphia: Lippincott Williams and Wilkins; 2010
- Foster C, Mistry NF, Peddi PF, Sharma S, eds. The Washington Manual of Medical Therapeutics. 33rd ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2010
- Gray J, ed. Therapeutic Choices. Canadian Pharmacists Association. 6th ed. Toronto: Webcom Inc. 2011
- Katzung BG, Masters SB, Trevor AJ, eds. Basic and Clinical Pharmacology. 11th ed. New York: McGraw-Hill; 2009
- Longo D, Fauci A, Kasper D, et al (eds). Harrison’s Principles of Internal Medicine. 18thed. New York: McGraw-Hill; 2011
- McPhee SJ, Papadakis MA, eds. Current Medical Diagnosis & Treatment. 49th ed. New York: McGraw-Hill; 2010
- Pagana KD, Pagana TJ eds. Mosby’s Diagnostic and Laboratory Test Reference. 9th ed. St. Louis: Elsevier-Mosby; 2009
- Rowland LP et al. (2010) Merritt’s Neurology (9th ed.) Philadelphia: Lippincoot Williams and Wilkins
- Skidmore-Roth L. ed. Mosby’s drug guide for nurses. 9th ed. St. Louis: Elsevier-Mosby; 2011
- Skidmore-Roth L, ed. Mosby’s nursing drug reference. 24th ed. St. Louis: Elsevier-Mosby; 2011
Online Pharmacological Resources:
- e-therapeutics
- Lexicomp
- RxList
- Epocrates Online
Journals/Clinical Trials:
- Andersson, PG, Hinge, HH, Johansen, O, et al. Double-blind study of naproxen vs placebo in the treatment of acute migraine attacks. Cephalalgia 1989; 9:29
- Ashina M, Saper J, Cady R et al. Eptinezumab in episodic migraine:A randomized, double-blind, placebo-controlled study (PROMISE-1) Cephalalgia 2020, 40(3) 241–254
- Cady R, Lipton RB, Hall C, et al. Treatment of mild headache in disabled migraine suffers Results of the Spectrum Study. Headache 2000; 40: 792-797
- Colman I et al. Parenteral dexamethasone for acute severe migraine headache: Meta-analysis of randomised controlled trials for preventing recurrence. BMJ 2008 Jun 14; 336:1359
- Croop R, Goadsby PJ, Stock DA et al. Efficacy, safety, and tolerability of rimegepant orally disintegrating tablet for the acute treatment of migraine: a randomised, phase 3, double-blind, placebo-controlled trial The Lancet, 2019; 394, P737-745
- Dodick DW, Lipton RB, Ailani J, et al. Ubrogepant for the Treatment of Migraine 2019 N Engl J Med 2019; 381:2230-2241 DOI: 10.1056/NEJMoa1813049
- Diener HC, Barbanti P, Dahlöf C, et al. BI 44370 TA, an oral CGRP antagonist for the treatment of acute migraine attacks: results from a phase II study. J.Cephalalgia. 2011 Apr; 31(5):573-84. Epub 2010 Dec 20
- Dahlof, C, Bjorkman, R. Diclofenac-K (50 and 100 mg) and placebo in the acute treatment of migraine. Cephalalgia 1993; 13:117
- Evans RW. Treating migraine in the emergency department. BMJ 2008 Jun 14; 336:1320
- Goadsby PJ, Reuter U, Hallström Y et al. A Controlled Trial of Erenumab for Episodic Migraine N Engl J Med 2017; 377:2123-2132 ; DOI: 10.1056/NEJMoa1705848
- Harriott AM, Takizawa1 T, Chung DY et al. Spreading depression as a preclinical model of migraine. The Journal of Headache and Pain. 2019; 20:45
- Havanka-Kanniainen, H. Treatment of acute migraine attack: ibuprofen and placebo compared. Headache 1989; 29:507
- Hewitt DJ, Aurora SK, Dodick DW, Randomized controlled trial of the CGRP receptor antagonist MK-3207 in the acute treatment of migraine. Cephalalgia. 2011 Apr; 31(6):712-22 Phase II b
- Kellstein, DE, Lipton, RB, Geetha, R, et al. Evaluation of a novel solubilized formulation of ibuprofen in the treatment of migraine headache: a randomized, double-blind, placebo-controlled, dose-ranging study. Cephalalgia 2000; 20:233
- Lipton RB, Stewart WF, Cady R. et al. 2000 Wolff Award. Sumatriptan for the range of headaches in migraine Sufferers. Results of the spectrum study. Headache 2000; 40: 783-91
- Liu F, Ma TB , Che X et al. The Efficacy of Venlafaxine, Flunarizine, and Valproic acid in the Prophylaxis of Vestibular Migraine. Frontiers in neurology 2017, 8: 524 ; doi.org/10.3389/fneur.2017.00524
- Massiou, H, Serrurier, D, Lasserre, O, Bousser, MG. Effectiveness of oral diclofenac in the acute treatment of common migraine attacks: a double-blind study versus placebo. Cephalalgia 1991; 11:59
- Nestvold, K, Kloster, R, Partinen, M, Sulkava,R. Treatment of acute migraine attack: naproxen and placebo compared. Cephalalgia 1985; 5:115
- Ramadan NM, Current Trends in Migraine Prophylaxis. Headache 2007;47]:S52-S57)
- Rose FC, et al. Pathogenesis of migraine. Journal of the Royal Society of Medicine.1991 84: 519-521
- Stauffer VL, Dodick DW, Zhang Q et al. Evaluation of Galcanezumab for the Prevention of Episodic Migraine: The EVOLVE-1 Randomized Clinical Trial. JAMA Neurol. 2018;75(9):1080-1088
- Shaunak S, Wilkins A, Pilling J B, Dick D J Pericardial, retroperitoneal, and pleural fibrosis induced by pergolide J Neurol Neurosurg Psychiatry 1999;66:79-81
- Singhal AB, Cerebral Vasoconstriction Syndromes. Top Stroke Rehabil 2004; 11:1-6
- The Diclofenac-K/Sumatriptan Migraine Study Group.Bussone G, Grazzi L, D’Amico D et al. Acute treatment of migraine attacks: efficacy and safety of a nonsteroidal anti-inflammatory drug, diclofenac-potassium, in comparison to oral sumatriptan and placebo Cephalalgia 1999; 4: 232-240
- VanderPluym , Dodick DW, Lipton RB et al. Fremanezumab for preventive treatment of migraine: Functional status on headache-free days Neurology 2018;91:e1152-e1165. doi:10.1212/01.wnl.0000544321.19316.40
- Welch, KM. Drug therapy of migraine. N Engl J Med 1993; 329:1476. Kloster, R, Nestvold, K, Vilming, ST. A double-blind study of ibuprofen versus placebo in the treatment of acute migraine attacks. Cephalalgia 1992; 12:169